March 09, 2022 | Deborah Kotz

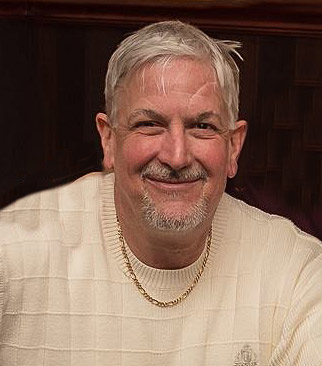
David Bennett, Sr., the 57 year old patient with terminal heart disease who made history as the first person to receive a genetically modified pig’s heart, passed away yesterday on March 8. Mr. Bennett received the transplant on January 7 and lived for two months following the surgery. His condition began deteriorating several days ago. After it became clear that he would not recover, he was given compassionate palliative care. He was able to communicate with his family during his final hours.
 “We are devastated by the loss of Mr. Bennett. He proved to be a brave and noble patient who fought all the way to the end. We extend our sincerest condolences to his family,” said Bartley P. Griffith, MD, who surgically transplanted the pig heart into the patient at the University of Maryland Medical Center (UMMC). Dr. Griffith is the Thomas E. and Alice Marie Hales Distinguished Professor in Transplant Surgery and Clinical Director of the Cardiac Xenotransplantation Program at the University of Maryland School of Medicine (UMSOM). “Mr. Bennett became known by millions of people around the world for his courage and steadfast will to live.”
“We are devastated by the loss of Mr. Bennett. He proved to be a brave and noble patient who fought all the way to the end. We extend our sincerest condolences to his family,” said Bartley P. Griffith, MD, who surgically transplanted the pig heart into the patient at the University of Maryland Medical Center (UMMC). Dr. Griffith is the Thomas E. and Alice Marie Hales Distinguished Professor in Transplant Surgery and Clinical Director of the Cardiac Xenotransplantation Program at the University of Maryland School of Medicine (UMSOM). “Mr. Bennett became known by millions of people around the world for his courage and steadfast will to live.”
 Muhammad M. Mohiuddin, MD, Professor of Surgery and Scientific Director of the Cardiac Xenotransplantation Program at UMSOM, added: “We are grateful to Mr. Bennett for his unique and historic role in helping to contribute to a vast array of knowledge to the field of xenotransplantation.”
Muhammad M. Mohiuddin, MD, Professor of Surgery and Scientific Director of the Cardiac Xenotransplantation Program at UMSOM, added: “We are grateful to Mr. Bennett for his unique and historic role in helping to contribute to a vast array of knowledge to the field of xenotransplantation.”
Mr. Bennett first came to UMMC as a patient in November 2021, where he was bedridden and placed on a heart-lung bypass machine, called extracorporeal membrane oxygenation (ECMO), to remain alive. He was deemed ineligible for a conventional heart transplant. Before consenting to receive the transplant, Mr. Bennett, was fully informed of the procedure’s risks, and that the procedure was experimental with unknown risks and benefits. On December 31, the US Food and Drug Administration granted an emergency authorization for the surgery in the hope of saving his life.
Following surgery, the transplanted heart performed very well for several weeks without any signs of rejection. The patient was able to spend time with his family and participate in physical therapy to help regain strength. He watched the Super Bowl with his physical therapist and spoke often about wanting to get home to his dog Lucky.
 “We have gained invaluable insights learning that the genetically modified pig heart can function well within the human body while the immune system is adequately suppressed,” said Dr. Mohiuddin. “We remain optimistic and plan on continuing our work in future clinical trials.”
“We have gained invaluable insights learning that the genetically modified pig heart can function well within the human body while the immune system is adequately suppressed,” said Dr. Mohiuddin. “We remain optimistic and plan on continuing our work in future clinical trials.”
Added Dr. Griffith: “As with any first-in-the-world transplant surgery, this one led to valuable insights that will hopefully inform transplant surgeons to improve outcomes and potentially provide lifesaving benefits to future patients.”
Statement from patient’s son, David Bennett, Jr., family spokesperson
We are profoundly grateful for the life-extending opportunity provided to my father, David Bennett Sr. by Dr. Griffith, Dr. Mohiuddin, Dr. Alison Grazioli and the stellar team at the University of Maryland School of Medicine and the University of Maryland Medical Center. Their exhaustive efforts and energy, paired with my dad’s insatiable will to live, created a hopeful environment during an uphill climb. Up until the end, my father wanted to continue fighting to preserve his life and spend more time with his beloved family, including his two sisters, his two children, and his five grandchildren, and his cherished dog Lucky. We were able to spend some precious weeks together while he recovered from the transplant surgery, weeks we would not have had without this miraculous effort.
 We have felt the prayers of the world during this time and humbly ask that those prayers continue to be offered on behalf of the medical teams, technology companies, research labs, grant writers and innovative initiatives of the future. We hope this story can be the beginning of hope and not the end. We also hope that what was learned from his surgery will benefit future patients and hopefully one day, end the organ shortage that costs so many lives each year.
We have felt the prayers of the world during this time and humbly ask that those prayers continue to be offered on behalf of the medical teams, technology companies, research labs, grant writers and innovative initiatives of the future. We hope this story can be the beginning of hope and not the end. We also hope that what was learned from his surgery will benefit future patients and hopefully one day, end the organ shortage that costs so many lives each year.
We are grateful for every innovative moment, every crazy dream, every sleepless night that went into this historic effort. We pray that those looking for hope will continue to fight for the future, fight for new ideas, fight for answers, fight for life. Fight like Dave.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 46 academic departments, centers, institutes, and programs, and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.2 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically based care for nearly 2 million patients each year. The School of Medicine has nearly $600 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 students, trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of over $6 billion and an economic impact of nearly $20 billion on the state and local community. The School of Medicine, which ranks as the 8th highest among public medical schools in research productivity (according to the Association of American Medical Colleges profile) is an innovator in translational medicine, with 606 active patents and 52 start-up companies. In the latest U.S. News & World Report ranking of the Best Medical Schools, published in 2021, the UM School of Medicine is ranked #9 among the 92 public medical schools in the U.S., and in the top 15 percent (#27) of all 192 public and private U.S. medical schools. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
Resources for the Media:
Contact
Deborah Kotz
410-706-4255 or 410-504-0054 (cell)
dkotz@som.umaryland.edu
Bill Seiler
(410) 328-8919 or (410) 913-8464 (cell)
bseiler@umm.edu
Related stories

Wednesday, January 31, 2024
Renowned Surgeon Dr. Bartley Griffith Named Vice Chair for Innovation in UM School of Medicine’s Department of Surgery
University of Maryland School of Medicine (UMSOM) Department of Surgery Chair Christine Lau, MD, MBA, along with UMSOM Dean Mark T. Gladwin, MD, announced today the appointment of Bartley P. Griffith, MD, as the Department of Surgery’s first Vice Chair for Innovation. In this role, Dr. Griffith will nurture a culture of innovation, entrepreneurship, and collaboration in the Department, and expand the integration of related sciences into surgical practice. The appointment is effective on February 1.

Friday, September 22, 2023
UM Medicine Faculty-Scientists and Clinicians Perform Second Historic Transplant of Pig Heart into Patient with End-Stage Cardiovascular Disease
A 58-year-old patient with terminal heart disease became the second patient in the world to receive a historic transplant of a genetically-modified pig heart on September 20. He is recovering and communicating with his loved ones. This is only the second time in the world that a genetically modified pig heart has been transplanted into a living patient. Both historic surgeries were performed by University of Maryland School of Medicine (UMSOM) faculty at the University of Maryland Medical Center (UMMC).

Friday, June 30, 2023
Lessons Learned from World’s First Successful Transplant of Genetically-Modified Pig Heart into Human Patient
A new study published today in the Lancet has revealed the most extensive analysis to date on what led to the eventual heart failure in the world's first successful transplant of a genetically-modified pig heart into a human patient. This groundbreaking procedure was conducted by University of Maryland School of Medicine (UMSOM) physician-scientists back in January 2022 and marked an important milestone for medical science.

Friday, May 28, 2021
Grateful Patient David Carroll Makes a $1 Million Bequest Pledge to Support the Future of the Advanced Heart Failure Program
University of Maryland School of Medicine (UMSOM) Dean E. Albert Reece, MD, PhD, MBA, announced today that grateful patient David Carroll has made a generous $1 million bequest pledge in support of the Advanced Heart Failure (AHF) program in UMSOM’s Department of Medicine’s Division of Cardiovascular Medicine. This gift follows an initial five-year pledge of $5,000 made by Mr. Carroll in 2017 for operating support of the program.

Wednesday, August 23, 2017
New Use of Blood Cleaning Device Saves High-Risk Patients With Liver Failure
Severe acute liver failure (ALF), a rare but life-threatening illness, is associated with high death rates if patients don’t receive timely treatment or a liver transplant. Unlike the heart or the kidneys, there is no established mechanical device to replace the liver’s function. Now, University of Maryland School of Medicine (UM SOM) researchers report that a device that removes toxins from the blood can also effectively provide a bridge to liver transplantation or buy time for a traumatically injured liver to heal, suggesting broader uses for the device than previously thought.

Friday, June 24, 2016
Surgical First: Patient Avoids Dialysis Thanks to Simultaneous Polycystic Kidney Removal and Kidney Transplant During 28-Person Kidney Swap
In a first-of-its-kind procedure in the United States, a patient was able to avoid dialysis when surgeons simultaneously removed two diseased kidneys and also transplanted a kidney from a living donor – all as part of a 28-person paired kidney exchange (PKE). The procedure, performed in May on a patient with polycystic kidney disease (PKD), eliminated the need for the patient to ever undergo dialysis.
