October 21, 2021 | Vanessa McMains
UM School of Medicine study in mice suggests it may be possible to develop treatments for various medical conditions caused by air pollution
Researchers have long known that air pollution can increase the risk of disorders such as obesity, diabetes, and fertility, but they did not know the exact mechanism for how it can lead to these health conditions.
Now, University of Maryland School of Medicine (UMSOM) researchers have shown how air pollution reduces sperm count in mice by causing inflammation in the brain.
 Scientists already know that the brain has a direct line to the reproductive organs affecting fertility and sperm count under stressful conditions. For example, emotional stress can lead to skipped menstrual periods in women. However, this latest study, published on Sept. 8 in Environmental Health Perspectives, connects the dots on how breathing polluted air can lower fertility.
Scientists already know that the brain has a direct line to the reproductive organs affecting fertility and sperm count under stressful conditions. For example, emotional stress can lead to skipped menstrual periods in women. However, this latest study, published on Sept. 8 in Environmental Health Perspectives, connects the dots on how breathing polluted air can lower fertility.
“Our findings showed that the damage due to air pollution—at least to the sperm count—could be remedied by removing a single inflammation marker in the brains of mice, suggesting that we may be able to develop therapies that could prevent or reverse the damaging effects of air pollution on fertility,” said lead study author Zhekang Ying, PhD, Assistant Professor of Medicine at UMSOM.
 Charles Hong, MD, PhD, the Melvin Sharoky, MD Professor in Medicine and Director of Cardiology Research at UMSOM said, “These findings have wider implications than just fertility, as there are many conditions, such as high blood pressure, diabetes, and heart disease that can result from brain inflammation due to air pollution.”
Charles Hong, MD, PhD, the Melvin Sharoky, MD Professor in Medicine and Director of Cardiology Research at UMSOM said, “These findings have wider implications than just fertility, as there are many conditions, such as high blood pressure, diabetes, and heart disease that can result from brain inflammation due to air pollution.”
About 92 percent of the world population lives in areas where the level of fine particles in the air smaller than 2.5 micrometers in diameter exceed the minimum safety standards set by the World Health Organization. These particles can come from sources such as car exhaust, factory emissions, wildfires, and woodburning stoves.
In past studies, some results have shown that mice exposed to air pollution did not always have inflammation of the testes —the male sex organs that make sperm — meaning that some other mechanism was potentially responsible for reduced sperm counts. Knowing the direct link between the brain and the sex organs, the researchers tested whether air pollution increased inflammation in the brain.
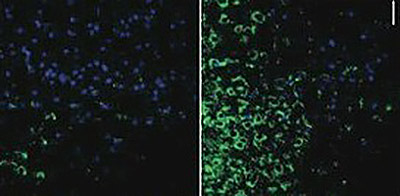 For this new study, researchers tested healthy mice and mice bred to lack a marker of inflammation in the brain, called Inhibitor Kappa B Kinase 2, or IKK2 for short, specifically located in the brain’s neurons. They exposed both healthy and IKK2 mutant mice to filtered air or air pollution and then tested their sperm counts. The mice bred without the IKK2 inflammation marker in their neurons did not have reductions in their sperm counts when exposed to the polluted air, unlike the healthy mice.
For this new study, researchers tested healthy mice and mice bred to lack a marker of inflammation in the brain, called Inhibitor Kappa B Kinase 2, or IKK2 for short, specifically located in the brain’s neurons. They exposed both healthy and IKK2 mutant mice to filtered air or air pollution and then tested their sperm counts. The mice bred without the IKK2 inflammation marker in their neurons did not have reductions in their sperm counts when exposed to the polluted air, unlike the healthy mice.
Researchers then removed IKK2 from specific neurons to determine more precisely how air pollution was leading to lower sperm counts. They found that one specific kind of neuron typically associated with sleep cycle and obesity was responsible for the reduced sperm count due to air pollution. These neurons typically are found in the hypothalamus, a part of the brain which controls hunger, thirst, and sex drive. The hypothalamus also works with the brain’s pituitary gland, which makes hormones that communicate directly with reproductive organs.
“Looking back, it makes perfect sense that the neurons in the hypothalamus are the culprits perpetuating this inflammation response that results in low sperm count, as we know that the hypothalamus is a major pathway link between the brain and the reproductive system,” said Dr. Ying.
 Albert Reece, MD, PhD, MBA, Executive Vice President for Medical Affairs, UM Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor and Dean at UMSOM commented, “ Environmental pollution is a problem of equity in that some persons who are poor or of color tend to face more severe health-related conditions due to greater exposure. It is important to explore the mechanisms by which pollution affects the body, so we can devise ways to prevent or treat these conditions to eliminate these health disparities.”
Albert Reece, MD, PhD, MBA, Executive Vice President for Medical Affairs, UM Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor and Dean at UMSOM commented, “ Environmental pollution is a problem of equity in that some persons who are poor or of color tend to face more severe health-related conditions due to greater exposure. It is important to explore the mechanisms by which pollution affects the body, so we can devise ways to prevent or treat these conditions to eliminate these health disparities.”
The study was funded by the National Institute of Environmental Health Sciences (R01ES024516, R01ES032290), the American Heart Association (13SDG17070131), National Natural Science Foundation of China (81302452), Major Projects of Natural Sciences of University in Jiangsu Province of China (18KJB330004), a project fund of Basic Scientific Research program of Nantong City (JC2019021), and Nantong University.
The researchers have no conflicts to report.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 46 academic departments, centers, institutes, and programs, and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.2 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically based care for nearly 2 million patients each year. The School of Medicine has nearly $600 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 students, trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of over $6 billion and an economic impact of nearly $20 billion on the state and local community. The School of Medicine, which ranks as the 8th highest among public medical schools in research productivity (according to the Association of American Medical Colleges profile) is an innovator in translational medicine, with 606 active patents and 52 start-up companies. In the latest U.S. News & World Report ranking of the Best Medical Schools, published in 2021, the UM School of Medicine is ranked #9 among the 92 public medical schools in the U.S., and in the top 15 percent (#27) of all 192 public and private U.S. medical schools. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
Contact
Vanessa McMains
Director, Media & Public Affairs
University of Maryland School of Medicine
Institute of Human Virology
vmcmains@ihv.umaryland.edu
Cell: 443-875-6099
Related stories
Wednesday, May 10, 2023
Research Identifies New Cause of Heart Failure Condition in Children
In an effort to determine the cause behind a rare condition that causes heart failure in children, University of Maryland School of Medicine researchers have identified new gene mutations responsible for the disorder in an infant patient. They were then able to learn how the mutation works and used a drug to reverse its effects in heart muscle cells derived from stem cells from the patient.
Friday, April 09, 2021
Researchers Link Several Heart Disease Risk Factors to Increased Risk of COVID-19 Infections
As the COVID-19 pandemic lingers, researchers have found associations between certain lifestyle factors and a person’s risk of getting infected. While it has already been established that those with Type II diabetes and a high body mass index (BMI) are at greater risk of experiencing hospitalizations and other severe complications related to COVID-19, they are also at greater risk of getting symptomatic infection in the first place. That is the finding of a recent study conducted by researchers at the University of Maryland School of Medicine (UMSOM)that was published in the journal, PLoS ONE.
Tuesday, October 15, 2019
Theme of 'Courage, Hope and Faith' Highlights Investiture of Dr. Charles Hong as the Melvin Sharoky, MD, Professor of Medicine
In a moving address to an audience of family members, UMSOM faculty and staff, and distinguished invited guests, Charles Hong, MD, PhD, echoed a theme that was heard throughout the ceremony of his investiture as the Melvin Sharoky, MD, Professor of Medicine: “Courage, Hope and Faith.”