March 29, 2021 | Vanessa McMains
Discovery Opens Door to Testing More Effective Drugs for Treating COVID-19 Patients
University of Maryland School of Medicine (UMSOM) researchers have identified the most toxic proteins made by SARS-COV-2—the virus that causes COVID-19 – and then used an FDA-approved cancer drug to blunt the viral protein’s detrimental effects. In their experiments in fruit flies and human cell lines, the team discovered the cell process that the virus hijacks, illuminating new potential candidate drugs that could be tested for treating severe COVID-19 disease patients. Their findings were published in two studies simultaneously on March 25 in Cell & Bioscience, a Springer Nature journal.
“Our work suggests there is a way to prevent SARS-COV-2 from injuring the body’s tissues and doing extensive damage,” says senior author of the study Zhe “Zion” Han, PhD, Associate Professor of Medicine and Director of the Center for Precision Disease Modeling at UMSOM. He notes that the most effective drug against Covid-19, remdesivir, only prevents the virus from making more copies of itself, but it does not protect already infected cells from damage caused by the viral proteins.
Prior to the pandemic, Dr. Han had been using fruit flies as a model to study other viruses, such as HIV and Zika. He says his research group shifted gears in February 2020 to study SARS-COV-2 when it was clear that the pandemic was going to significantly impact the U.S.
SARS-COV-2 infects cells and hijacks them into making proteins from each of its 27 genes. Dr. Han’s team introduced each of these 27 SARS-CoV-2 genes in human cells and examined their toxicity. They also generated 12 fruit fly lines to express SARS-CoV-2 proteins likely to cause toxicity based on their structure and predicted function.
The researchers found that a viral protein, known as Orf6, was the most toxic killing about half of the human cells. Two other proteins (Nsp6 and Orf7a) also proved toxic, killing about 30-40 percent of the human cells. Fruit flies that made any one of these three toxic viral proteins in their bodies were less likely to survive to adulthood. Those fruit flies that did live had problems like fewer branches in their lungs or fewer energy-generating power factories in their muscle cells.
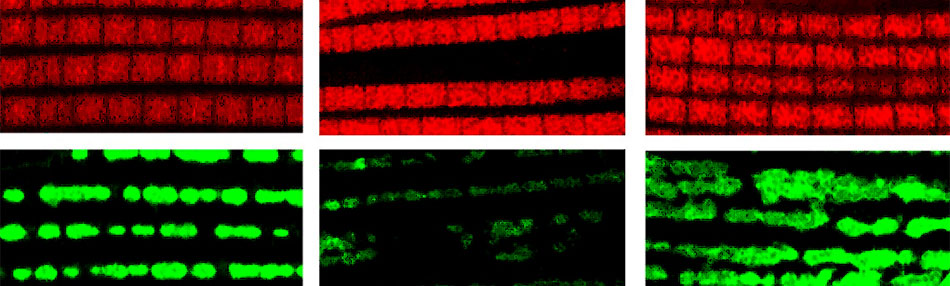 Healthy fruit fly muscles (left) have many energy-generating power factories (green). The fruit fly muscles that have the SARS-COV-2 Orf6 protein (center) produce fewer power factories, which are restored (right) when the flies are treated with the cancer drug selinexor. Caption: Dr. Zhe Han
Healthy fruit fly muscles (left) have many energy-generating power factories (green). The fruit fly muscles that have the SARS-COV-2 Orf6 protein (center) produce fewer power factories, which are restored (right) when the flies are treated with the cancer drug selinexor. Caption: Dr. Zhe Han
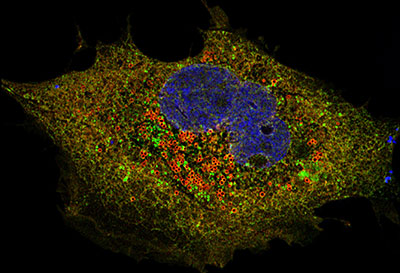
For the remaining experiments, the researchers focused on just the most toxic viral protein, so they could figure out what cell process the virus hijacks during infection. Dr. Han’s team found that the virus’ toxic Orf6 protein sticks to multiple human proteins that have the job of moving materials out of the cell’s nucleus—the place in the cell that holds the genome, or the instructions for life.
They then discovered that one of these human moving proteins, targeted by the virus, gets blocked by the cancer drug selinexor. The researchers tested selinexor on human cells and fruit flies making the toxic viral protein to see if the drug could help reverse the damage. Selinexor, like many cancer drugs is itself toxic. However, after accounting for its toxic effects, the drug improved human cell survival by about 12 percent. Selinexor prevented early death in about 15 percent of the flies making the toxic viral protein. The drug also restored branches in the lungs and the energy-generators in the muscle cells. Selinexor is FDA-approved to treat certain blood cancers.
More than 1,000 FDA-approved drugs are in clinical trials to test as treatments for Covid-19, and luckily a trial testing selinexor, the drug used in our study, is being performed already,” says Dr. Han. “If this trial proves to be successful, our data will have demonstrated the underlying mechanism for why the drug works.”
E. Albert Reece, MD, PhD, MBA, Executive Vice President for Medical Affairs, University of Maryland Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor and Dean, University of Maryland School of Medicine, commented, “Although we now have vaccines, it may still be a while before we will have Covid-19 infections under control, especially with the new variants emerging. We will need to tap into every tool in the arsenal available to protect people from needless sickness, disability or even death, and this study guides us towards a new target for potential therapeutics.”
 These two studies were funded by a University of Maryland COVID-19 Accelerated Translational Incubator Pilot Grant, the University of Maryland, the Baltimore Institute for Clinical and Translational Research, and the University of Maryland School of Pharmacy Mass Spectrometry Center.
These two studies were funded by a University of Maryland COVID-19 Accelerated Translational Incubator Pilot Grant, the University of Maryland, the Baltimore Institute for Clinical and Translational Research, and the University of Maryland School of Pharmacy Mass Spectrometry Center.
The researchers do not have any conflicts of interest to report.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 46 academic departments, centers, institutes, and programs, and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.2 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically based care for nearly 2 million patients each year. The School of Medicine has nearly $600 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 students, trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of over $6 billion and an economic impact of nearly $20 billion on the state and local community. The School of Medicine, which ranks as the 8th highest among public medical schools in research productivity (according to the Association of American Medical Colleges profile) is an innovator in translational medicine, with 606 active patents and 52 start-up companies. In the latest U.S. News & World Report ranking of the Best Medical Schools, published in 2021, the UM School of Medicine is ranked #9 among the 92 public medical schools in the U.S., and in the top 15 percent (#27) of all 192 public and private U.S. medical schools. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
Contact
Vanessa McMains, PhD
Director of Media & Public Affairs
Institute for Human Virology
University of Maryland School of Medicine
Phone: 443-875-6099
Email: vmcmains@ihv.umaryland.edu
Related stories

Monday, February 02, 2026
University of Maryland School of Medicine Launches Clinical Trial of Investigative Nasal Spray Medicine to Prevent Illnesses from Respiratory Viruses
Last year, at least one million people in the U.S. were hospitalized for respiratory virus illnesses like the flu or COVID-19, according to the Centers for Disease Control and Prevention. Many of these individuals were at higher risk of getting infections due to living or working around young children who contract more respiratory infections. A new clinical trial led by researchers at the University of Maryland School of Medicine’s (UMSOM) Center for Vaccine Development and Global Health (CVD) will test a new experimental intranasal spray designed to boost immune defenses and reduce illness from respiratory viruses.
Wednesday, March 20, 2024
New Study Reveals Insights into Lack of Durability in COVID Antibody Response to Infections & Vaccines
Researchers at the Institute of Human Virology (IHV) at the University of Maryland School of Medicine published a new study in the Journal of Infectious Diseases investigating the short-lived antibody response following SARS-CoV-2, the virus that causes COVID.

Thursday, January 21, 2021
UM School of Medicine Hosted Media Availability for Ensuring Trust in COVID-19 Vaccine Event
On January 22, 2021 at 2 p.m., the University of Maryland School of Medicine (UMSOM) hosted Black faith-based leaders, COVID-19 research volunteers, and “America’s Doctor,” Anthony Fauci, MD. The event provided straight talk about fears, trust issues, and why we need our Black and Brown community to be a part of COVID-19 vaccine research.

Tuesday, December 22, 2020
Largest Study of Its Kind Identifies Which COVID-19 Patients Face the Greatest Risk of Mortality During Hospitalization
Hospitalized COVID-19 patients have a greater risk of dying if they are men or if they are obese or have complications from diabetes or hypertension, according to a new study conducted by University of Maryland School of Medicine (UMSOM) researchers. In a study published in the journal Clinical Infectious Diseases, the researchers evaluated nearly 67,000 hospitalized COVID-19 patients in 613 hospitals across the country to determine the link between certain common patient characteristics and the risk of dying from COVID-19. Their analysis found that men had a 30 percent higher risk of dying compared to women of the same age and health status. Hospitalized patients who were obese, had hypertension or poorly managed diabetes had a higher risk of dying compared to those who did not have these conditions. Those aged 20 to 39 with these conditions had the biggest difference in their risk of dying compared to their healthier peers.

Thursday, October 22, 2020
New Landmark Study at UM School of Medicine Finds Aspirin Use Reduces Risk of Death in Hospitalized COVID-19 Patients
Hospitalized COVID-19 patients who were taking a daily low-dose aspirin to protect against cardiovascular disease had a significantly lower risk of complications and death compared to those who were not taking aspirin, according to a new study led by researchers at the University of Maryland School of Medicine (UMSOM). Aspirin takers were less likely to be placed in the intensive care unit (ICU) or hooked up to a mechanical ventilator, and they were more likely to survive the infection compared to hospitalized patients who were not taking aspirin, The study, published today in the journal Anesthesia and Analgesia, provides “cautious optimism,” the researchers say, for an inexpensive, accessible medication with a well-known safety profile that could help prevent severe complications.

Tuesday, June 16, 2020
UM School of Medicine Researchers Receive Federal Funding to Rapidly Test New Treatments for COVID-19
Researchers at the University of Maryland School of Medicine (UMSOM) will be partnering on an agreement funded by the federal government’s Defense Advanced Research Projects Agency (DARPA) to rapidly test hundreds of drugs, approved and marketed for other conditions, to see whether any can be repurposed to prevent or treat COVID-19. The compounds will be tested in studies using state-of-the-art technologies in the laboratory of coronavirus researcher Matthew Frieman, PhD., Associate Professor of Microbiology and Immunology at the University of Maryland School of Medicine. UMSOM will receive up to $3.6 million over the next year to fund this effort.
Monday, June 15, 2020
UM School of Medicine Researchers Help Identify Potent Antibody Cocktail with Potential to Treat COVID-19
Researchers at the University of Maryland School of Medicine (UMSOM) evaluated several human antibodies to determine the most potent combination to be mixed in a cocktail and used as a promising anti-viral therapy against the virus that causes COVID-19. Their research, conducted in collaboration with scientists at Regeneron Pharmaceuticals, was published today in the journal Science. The study demonstrates the rapid process of isolating, testing and mass-producing antibody therapies against any infectious disease by using both genetically engineered mice and plasma from recovered COVID-19 patients.

Tuesday, June 02, 2020
UM School of Medicine’s Institute of Human Virology Awarded Grants to Strengthen COVID-19 Response in Sub-Saharan Africa
The Center for International Health, Education and Biosecurity (Ciheb) at the University of Maryland School of Medicine’s Institute of Human Virology was awarded $4 million from the U.S. Centers for Disease Control and Prevention (CDC) to support coronavirus disease 2019 (COVID-19) response activities in Botswana, Nigeria, Malawi, and Mozambique.

Friday, June 24, 2016
Surgical First: Patient Avoids Dialysis Thanks to Simultaneous Polycystic Kidney Removal and Kidney Transplant During 28-Person Kidney Swap
In a first-of-its-kind procedure in the United States, a patient was able to avoid dialysis when surgeons simultaneously removed two diseased kidneys and also transplanted a kidney from a living donor – all as part of a 28-person paired kidney exchange (PKE). The procedure, performed in May on a patient with polycystic kidney disease (PKD), eliminated the need for the patient to ever undergo dialysis.
