December 07, 2017 | David Kohn

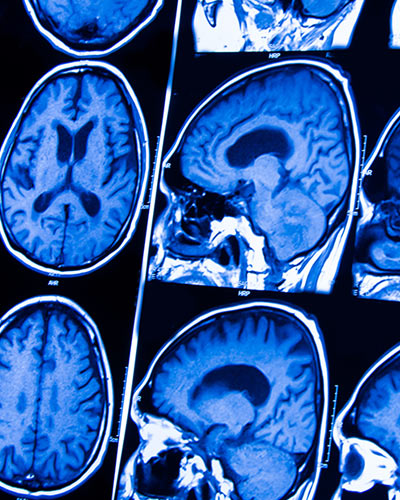
Two-Way Brain-Gut Interactions May Worsen Outcome After TBI
University of Maryland School of Medicine (UMSOM) researchers have found a two-way link between traumatic brain injury (TBI) and intestinal changes. These interactions may contribute to increased infections in these patients, and may also worsen chronic brain damage.
This is the first study to find that TBI in mice can trigger delayed, long-term changes in the colon and that subsequent bacterial infections in the gastrointestinal system can increase posttraumatic brain inflammation and associated tissue loss. The findings were published recently in the journal Brain, Behavior, and Immunity.
“These results indicate strong two-way interactions between the brain and the gut that may help explain the increased incidence of systemic infections after brain trauma and allow new treatment approaches,” said the lead researcher, Alan Faden, MD, the David S. Brown Professor in Trauma in the Departments of Anesthesiology, Anatomy & Neurobiology, Psychiatry, Neurology, and Neurosurgery at UMSOM, and director of the UMSOM Shock, Trauma and Anesthesiology Research Center.
Researchers have known for years that TBI has significant effects on the gastrointestinal tract, but until now, scientists have not recognized that brain trauma can make the colon more permeable, potentially allowing allow harmful microbes to migrate from the intestine to other areas of the body, causing infection.. People are 12 times more likely to die from blood poisoning after TBI, which is often caused by bacteria, and 2.5 times more likely to die of a digestive system problem, compared with those without such injury.
 In this study, the researchers examined mice that received an experimental TBI. They found that the intestinal wall of the colon became more permeable after trauma, changes that were sustained over the following month.
In this study, the researchers examined mice that received an experimental TBI. They found that the intestinal wall of the colon became more permeable after trauma, changes that were sustained over the following month.
It is not clear how TBI causes these gut changes. A key factor in the process may be enteric glial cells (EGCs), a class of cells that exist in the gut. These cells are similar to brain astroglial cells, and both types of glial cells are activated after TBI. After TBI, such activation is associated with brain inflammation that contributes to delayed tissue damage in the brain. Researchers don’t know whether activation of ECGs after TBI contributes to intestinal injury or is instead an attempt to compensate for the injury.
The researchers also focused on the two-way nature of the process: how gut dysfunction may worsen brain inflammation and tissue loss after TBI. They infected the mice with Citrobacter rodentium, a species of bacteria that is the rodent equivalent of E. coli, which infects humans. In mice with a TBI who were infected with this the bacteria, brain inflammation worsened. Furthermore, in the hippocampus, a key region for memory, the mice who had TBI and were then infected lost more neurons than animals without infection.
This suggests that TBI may trigger a vicious cycle, in which brain injury causes gut dysfunction, which then has the potential to worsen the original brain injury. “These results really underscore the importance of bi-directional gut-brain communication on the long-term effects of TBI,” said Dr. Faden.
Other authors of this paper include Elise Ma, a doctoral student; Terez Shea-Donahue PhD, professor of radiation oncology; Bogdan A. Stoica, MD, associate professor of anesthesiology ; and David Loane, PhD, associate professor of anesthesiology- all at UMSOM.
“This research has the potential to eventually connect bench to bedside in a groundbreaking way,” said E. Albert Reece, MD, PhD, MBA, Executive Vice President for Medical Affairs at the University of Maryland and John Z. and Akiko K. Bowers Distinguished Professor and Dean of the University of Maryland School of Medicine. “Dr. Faden is part of a first-rate collection of scientists at the School who are unraveling the complexities of traumatic brain injury and its effects on the body.”
About the University of Maryland School of Medicine
Commemorating its 210th Anniversary, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 43 academic departments, centers, institutes, and programs; and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Sciences, and a distinguished recipient of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically-based care for more than 1.2 million patients each year. The School has over 2,500 students, residents, and fellows, and nearly $450 million in extramural funding, with more than half of its academic departments ranked in the top 20 among all public medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total workforce of nearly 7,000 individuals. The combined School and Medical System (“University of Maryland Medicine”) has a total budget of $5 billion and an economic impact of nearly $15 billion on the state and local community. The School of Medicine faculty, which ranks as the 8th-highest public medical school in research productivity, is an innovator in translational medicine with 600 active patents and 24 start-up companies. The School works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu/
Learn More
Contact
Office of Public Affairs
655 West Baltimore Street
Bressler Research Building 14-002
Baltimore, Maryland 21201-1559
Contact Media Relations
(410) 706-5260
Related stories
Monday, January 27, 2020
UM School of Medicine's Shock, Trauma and Anesthesiology Research (STAR) Center Announces Leadership Transition
University of Maryland School of Medicine (UMSOM) Dean E. Albert Reece, MD, PhD, MBA, announced today that the UMSOM”s Shock, Trauma and Anesthesiology Research (STAR) Center will begin the next phase of its history with new leadership.

Friday, November 22, 2019
UM School of Medicine Marks 10th Anniversary of Shock Trauma and Anesthesiology Research (STAR) Center
The Shock Trauma and Anesthesiology Research (STAR) Center at the University of Maryland School of Medicine (UMSOM), one of the first centers in the U.S. dedicated exclusively to studying the prevention and treatment of trauma, held a full-day symposium to mark the Research Center’s 10-year anniversary. Over the past decade, the world-class, multi-disciplinary research center has focused on traumatic brain injury, critical care, organ support, injury prevention, and surgical outcomes.
Monday, March 20, 2017
University of Maryland School of Medicine Researchers Identify New Pathway for Brain Inflammation
University of Maryland School of Medicine (UM SOM) researchers have identified a new mechanism by which inflammation can spread throughout the brain after injury. This mechanism may explain the widespread and long-lasting inflammation that occurs after traumatic brain injury, and may play a role in other neurodegenerative diseases.

Monday, December 05, 2016
UMSOM Neuroscientist, Dr. Alan Faden, to Lead Research Collaborations Across University Campuses
University of Maryland School of Medicine Dean E. Albert Reece announced today that Alan I. Faden, MD, the David S. Brown Professor in Trauma and Professor of Anesthesiology at the University of Maryland School of Medicine (UM SOM), and Director of the UM SOM Shock Trauma and Anesthesiology Research center (STAR), has been appointed to the new position of Associate Dean for Trans-Campus Research Advancement at the UM SOM.
