Brain-Systemic Interactions After TBI
Severe TBI patients have a hospital infection rate of ~50%, significantly higher than seen in stroke, polytrauma, and burn patients. Acute-onset pneumonia represents 30-50% of infections in severe TBI patients and leads to longer hospital stays and increased morbidity and mortality. Our lab is working on demonstrating the bidirectional effects of the brain and the lungs. Using a two hit model of TBI and subsequent bacterial lung infection, we can investigate the impact of pneumonia on TBI and vice versa. At 3 days and 60 days following TBI mice are administered a bacterial infection. Our lab has found that TBI causes increased mortality to bacterial infection and results in neuroinflammation and poor neurological outcome. Alternatively, in the lung, the peripheral immune response to infection is dysfunctional, resulting in increased bacterial burden and lung pathology. Currently, we are investigating the mechanism underlying these bidirectional effects and are hoping to provide new clinical targets to better outcomes for TBI survivors.
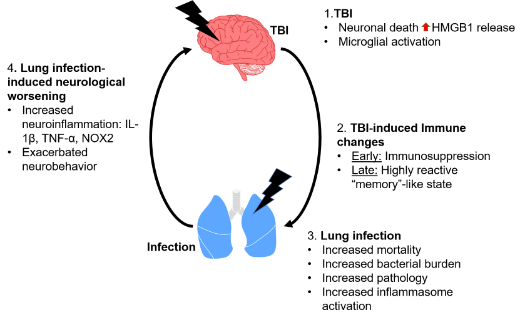
Figure 6.1 Model for bidirectional effects of TBI and lung-infection. When 1) TBI occurs this results in BBB damage and neuronal death, leading to the release of HMGB1 from dying neurons and activation of microglia. TBI results in 2) TBI-induced immune changes which we have described here as early immunosuppression of circulating monocytes and later as a more memory-like highly reactive state for circulating monocytes. At both timepoints when there is a 3) lung infection this results in a dysregulated immune response, leading to increased mortality, lung bacterial burden and pathology, potentially driven by inflammasome activation. Furthermore, 4) lung infection induces neurological worsening resulting in increased neuroinflammation and exacerbated behavioral responses.
