February 25, 2020 | Deborah Kotz
Preclinical Study Suggests Prolonged Inflammation After Brain Injury Can Be Reversed by Temporarily Depleting Immune Cells long after injury
Researchers at the University of Maryland School of Medicine (UMSOM) found that targeting overactive immune cells in the brain with an experimental drug could limit brain cell loss and reverse cognitive and motor difficulties caused by traumatic brain injury (TBI). The findings, published Monday in the Journal of Neuroscience, suggest a potential new treatment for TBI and possibly other brain injuries.

More importantly, the mice recovered markedly better than the control group that didn’t receive treatment, showing less loss of tissue and neurons with significantly better motor and cognitive performance.
“We were surprised to see that the extent to which such late treatment could reverse the inflammatory state and the cognitive effects of experimental TBI,” said study co-author Rebecca Henry, PhD, Research Associate in Anesthesiology at UMSOM. “This was a proof of concept study that depletion and subsequent repopulation of microglia cells after injury has a strong protective effect, but we clearly need more research to better understand this process before clinical translation.”
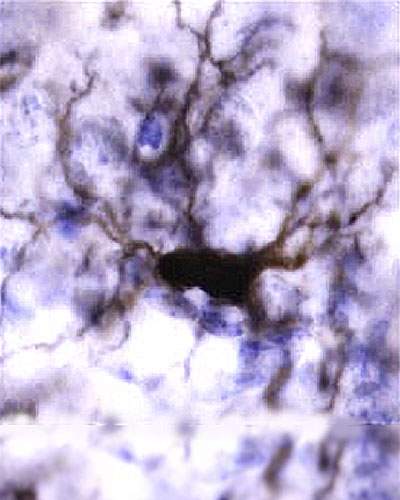
 Both human and animal brains have specialized immune cells, called microglia, that protect against bacteria or viruses that enter the brain.
Both human and animal brains have specialized immune cells, called microglia, that protect against bacteria or viruses that enter the brain.
Evidence from previous clinical studies has shown an increase in microglia activation in patients who have suffered a moderate or severe traumatic brain injury. These changes appear to be correlated with neurological deficits in such patients, including cognitive function.
“These preclinical studies suggest that the consequences of TBI on brain degeneration and related neurological impairment may be modifiable quite long after injury,” said study co-author Alan Faden, MD, the David S. Brown Professor in Trauma at UMSOM.
“We can potentially alter these effects by even highly delayed targeting of inflammatory pathways, a finding at odds with widely accepted views about treating head injury.”
The next step for the researchers is to isolate the microglia cells and use RNA resequencing techniques to learn more about which genes are driving inflammation and overactivation in order to better understand the mechanism identified in this study.
“This is an intriguing finding that points to an important role that inflammation plays in chronic debilitation from brain injuries,” said UMSOM Dean E. Albert Reece, MD, PhD, MBA, University Executive Vice President for Medical Affairs and the John Z. and Akiko K. Bowers Distinguished Professor. “Future studies will hopefully lead to new treatments for severe TBI that destroys a patient’s quality of life.”
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 45 academic departments, centers, institutes, and programs; and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.2 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically based care for nearly 2 million patients each year. The School of Medicine has more than $540 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 student trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of nearly $6 billion and an economic impact more than $15 billion on the state and local community. The School of Medicine faculty, which ranks as the 8th highest among public medical schools in research productivity, is an innovator in translational medicine, with 600 active patents and 24 start-up companies. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
Contact
Office of Public Affairs
655 West Baltimore Street
Bressler Research Building 14-002
Baltimore, Maryland 21201-1559
Contact Media Relations
(410) 706-5260
Deborah Kotz
Director of Media Relations
Office of Public Affairs & Communications
University of Maryland School of Medicine
o: 410-706-4255
c: 410-804-0054
t: @debkotz2
