March 20, 2017
Findings Could Transform How We Understand Brain Injury and Disease
University of Maryland School of Medicine (UM SOM) researchers have identified a new mechanism by which inflammation can spread throughout the brain after injury. This mechanism may explain the widespread and long-lasting inflammation that occurs after traumatic brain injury, and may play a role in other neurodegenerative diseases.
The findings were published recently in the Journal of Neuroinflammation.
This new understanding has the potential to transform how brain inflammation is understood, and, ultimately, how it is treated. The researchers focused on microparticles, pieces of cells that are released from certain brain immune cells following injury. Researchers have long known of microparticles but have only recently begun to focus on them as a messengers of inflammation and potentially key factors in brain disease. The researchers found that it may be possible to use the microparticles as biomarkers for brain inflammation, and in an animal model, have identified a potential method for reducing the effect of the microparticles on the brain.
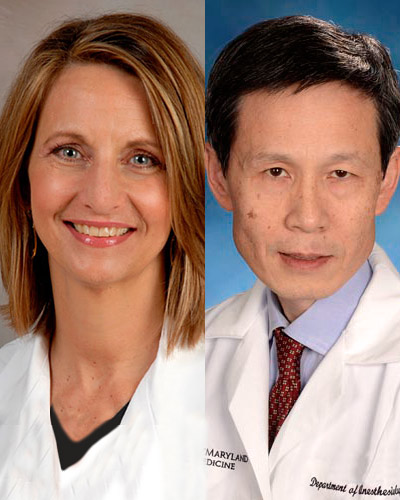
The researchers who are co-authors on this article include: Stephen R. Thom, MD, PhD, professor of emergency medicine at UM SOM; Alan Faden, MD, the David S. Brown Professor in the Departments of Anesthesiology, Anatomy & Neurobiology, Neurology, and Neurosurgery at UM SOM, and director of the UM SOM Shock, Trauma and Anesthesiology Research Center (STAR) as well as the National Study Center for Trauma and Emergency Medical Services, and associate dean of trans-campus research advancement; Bogdan A. Stoica, MD, associate professor of anesthesiology at UM SOM; and David Loane, PhD, an assistant professor of anesthesiology at UM SOM.




From Left to Right: Stephen R. Thom, MD, PhD, Alan Faden, MD, Bogdan A. Stoica, MD, and David Loane, PhD
“These results are really transformational,” said Dr. Faden. “This is a new field. The idea that inflammation can trigger more inflammation is really new, and really exciting.”
The researchers studied mice, and found that in animals who had a traumatic brain injury, levels of microparticles in the blood were much higher. Because each kind of cell in the body has a distinct fingerprint, the researchers could track exactly where the microparticles came from. The microparticles they looked at in this study are released from cells known as microglia, immune cells that are common in the brain. After an injury, these cells often go into overdrive in an attempt to fix the injury. However, this outsized response can often worsen inflammation.
Research has found that neuroinflammation goes on for years. The researchers say that microparticles may play a role in this process.
The findings have real-world implications. The researchers say that microparticles in the blood have the potential to be used as a biomarker – a way to determine how serious a brain injury is. This could help guide treatment of the injuries, whose severity is often difficult to gauge.
They also found that exposing the inflammatory microparticles to a compound called PEG-TB could neutralize them. This opens up the possibility of using that, or other compounds to treat TBI, or perhaps even other neurodegenerative diseases.
“Our understanding of brain injury is evolving very rapidly,” said University of Maryland School of Medicine Dean E. Albert Reece, MD, PhD, MBA, who is also the vice president for Medical Affairs, University of Maryland, and the John Z. and Akiko K. Bowers Distinguished Professor. “This finding by Dr. Faden and Dr. Loane is an exciting and unexpected step forward. It seems likely that it will eventually lead to more effective ways to evaluate and possibly treat patients with brain injury.”
About the University of Maryland School of Medicine
Celebrating its 210th Anniversary, the University of Maryland School of Medicine was chartered in 1807 and is the first public medical school in the United States and continues today as an innovative leader in accelerating innovation and discovery in medicine. The School of Medicine is the founding school of the University of Maryland and is an integral part of the 11-campus University System of Maryland. Located on the University of Maryland’s Baltimore campus, the School of Medicine works closely with the University of Maryland Medical Center and Medical System to provide a research-intensive, academic and clinically based education. With 43 academic departments, centers and institutes and a faculty of more than 3,000 physicians and research scientists plus more than $400 million in extramural funding, the School is regarded as one of the leading biomedical research institutions in the U.S. with top-tier faculty and programs in cancer, brain science, surgery and transplantation, trauma and emergency medicine, vaccine development and human genomics, among other centers of excellence. The School is not only concerned with the health of the citizens of Maryland and the nation, but also has a global presence, with research and treatment facilities in more than 35 countries around the world. medschool.umaryland.edu/
Learn More
• Department of Anatomy & Neurobiology
• Department of Anesthesiology
• Department of Neurosurgery
• Department of Emergency Medicine
Contact
Office of Public Affairs
655 West Baltimore Street
Bressler Research Building 14-002
Baltimore, Maryland 21201-1559
Contact Media Relations
(410) 706-5260
Related stories
Monday, January 27, 2020
UM School of Medicine's Shock, Trauma and Anesthesiology Research (STAR) Center Announces Leadership Transition
University of Maryland School of Medicine (UMSOM) Dean E. Albert Reece, MD, PhD, MBA, announced today that the UMSOM”s Shock, Trauma and Anesthesiology Research (STAR) Center will begin the next phase of its history with new leadership.

Friday, November 22, 2019
UM School of Medicine Marks 10th Anniversary of Shock Trauma and Anesthesiology Research (STAR) Center
The Shock Trauma and Anesthesiology Research (STAR) Center at the University of Maryland School of Medicine (UMSOM), one of the first centers in the U.S. dedicated exclusively to studying the prevention and treatment of trauma, held a full-day symposium to mark the Research Center’s 10-year anniversary. Over the past decade, the world-class, multi-disciplinary research center has focused on traumatic brain injury, critical care, organ support, injury prevention, and surgical outcomes.

Thursday, December 07, 2017
University of Maryland School of Medicine Scientists Find that Traumatic Brain Injury Causes Intestinal Damage
University of Maryland School of Medicine (UMSOM) researchers have found a two-way link between traumatic brain injury (TBI) and intestinal changes. These interactions may contribute to increased infections in these patients, and may also worsen chronic brain damage.

Monday, December 05, 2016
UMSOM Neuroscientist, Dr. Alan Faden, to Lead Research Collaborations Across University Campuses
University of Maryland School of Medicine Dean E. Albert Reece announced today that Alan I. Faden, MD, the David S. Brown Professor in Trauma and Professor of Anesthesiology at the University of Maryland School of Medicine (UM SOM), and Director of the UM SOM Shock Trauma and Anesthesiology Research center (STAR), has been appointed to the new position of Associate Dean for Trans-Campus Research Advancement at the UM SOM.
