March 14, 2016 | David Kohn

While the benefits of a good night’s sleep can be priceless, and sleeplessness imposes significant costs on the individual and society, little is known about the financial impact of treatment for sleep-related disorders. Sleep researchers at the University of Maryland School of Medicine, who conducted the first-ever review of insomnia treatment cost-effectiveness, found financial estimates of untreated sleeplessness in the United States topping $100 billion a year and studies documenting substantial healthcare cost savings when insomnia is treated, recouping treatment costs within six-to-12 months. Their analysis was published recently in the journal Sleep Medicine Reviews.
Roughly one out of five adults in the U.S. has difficulty falling asleep or staying asleep, according to the review’s lead author, Emerson M. Wickwire, PhD. “Insomnia is the most widespread clinical sleep disorder among adults. Sleep for some people is a lot like a slippery fish. The more you try to grab at it, the more it jumps out of your hands,” says Wickwire, an assistant professor of psychiatry and medicine at the University of Maryland School of Medicine and director of the Insomnia Program at the University of Maryland Medical Center.
The review found that the estimated financial costs of insomnia range from $28.1 billion to $216.6 billion. Wickwire and his team note that newer studies tend to report more comprehensive – and thus higher – estimates. The review found that much of insomnia’s economic toll is based on indirect costs: poorer workplace performance, higher health care utilization and increased accident risk. More recent studies have focused on the impact of insomnia on health-related quality of life – its effect on a person’s physical, emotional and social life, and overall happiness. The review found that people with insomnia consistently report lower quality of life scores compared to their non-insomniac peers.
Wickwire says highly effective drug-based and behavioral therapies for insomnia exist, but the majority of people with insomnia never receive treatment. “People don’t seek care in part because they’re uncomfortable acknowledging it’s a problem, or they don’t realize it’s a problem or that effective treatments are available. And, of course, there’s a gross lack of awareness among healthcare providers as well,” he says.
Wickwire says another key barrier is limited access to care: “Payers such as health insurers have historically underfunded insomnia treatment, in part because they have not been sure what the payoff is.”
The researchers reviewed 10 studies of the cost-effectiveness of both pharmacological and behavioral treatments. The review found that both medication and behavioral interventions were more than worth the money.
Wickwire says that treatment likely reduces overall healthcare use related to insomnia.
The authors suggest that insomnia researchers should measure direct and indirect insomnia-related costs in all their studies, including measures of workplace productivity and healthcare quality of life.
“Cost-effectiveness is a key part of current healthcare research,” says E. Albert Reece, MD, PhD, MBA, vice president for medical affairs at the University of Maryland and the John Z. and Akiko K. Bowers Distinguished Professor and dean of the University of Maryland School of Medicine. “This timely review presents information that may help policymakers determine the most effective, most efficient ways to improve the quality of sleep, which is a fundamental health requirement.”
Wickwire EM, Shaya FT, Scharf SM. “Health economics of insomnia treatments: The return on investment for a good night’s sleep.” Sleep Medicine Reviews, 30(2016):72-82.
About the University of Maryland School of Medicine
The University of Maryland School of Medicine was chartered in 1807 and is the first public medical school in the United States and continues today as an innovative leader in accelerating innovation and discovery in medicine. The School of Medicine is the founding school of the University of Maryland and is an integral part of the 11-campus University System of Maryland. Located on the University of Maryland’s Baltimore campus, the School of Medicine works closely with the University of Maryland Medical Center and Medical System to provide a research-intensive, academic and clinically based education. With 43 academic departments, centers and institutes and a faculty of more than 3,000 physicians and research scientists plus more than $400 million in extramural funding, the School is regarded as one of the leading biomedical research institutions in the U.S. with top-tier faculty and programs in cancer, brain science, surgery and transplantation, trauma and emergency medicine, vaccine development and human genomics, among other centers of excellence. The School is not only concerned with the health of the citizens of Maryland and the nation, but also has a global presence, with research and treatment facilities in more than 35 countries around the world. For more information, visit http://medschool.umaryland.edu.
About the University of Maryland Medical Center
The University of Maryland Medical Center (UMMC) is comprised of two hospitals in Baltimore: an 800-bed teaching hospital — the flagship institution of the 12-hospital University of Maryland Medical System (UMMS) — and a 200-bed community teaching hospital, UMMC Midtown Campus. UMMC is a national and regional referral center for trauma, cancer care, neurocare, cardiac care, diabetes and endocrinology, women's and children's health, and has one of the largest solid organ transplant programs in the country. All physicians on staff at the flagship hospital are faculty physicians of the University of Maryland School of Medicine. At UMMC Midtown Campus, faculty physicians work alongside community physicians to provide patients with the highest quality care. UMMC Midtown Campus was founded in 1881 and is located one mile away from the University Campus hospital. For more information, visit www.umm.edu.
Contact
Department of Anesthesiology
(410) 328-6120 (phone)
(410) 328-5531 (fax)
swalsh@som.umaryland.edu
David Kohn
Director of Medicine and Science Communications
University of Maryland School of Medicine
Office of Public Affairs
dkohn@som.umaryland.edu
(410) 706-7590
Related stories

Thursday, January 08, 2026
Improving Sleep Isn’t Enough: Researchers Highlight Daytime Function as Key to Assessing Insomnia Treatments
About one in nine adults suffer from chronic insomnia and its residual effects like drowsiness, cognitive issues, and irritability as well as increased health risks like diabetes and heart risks if left untreated. While many treatments are available, the challenge lies in determining how well a medication or other sleep aid works in individual patients.

Monday, June 30, 2025
UM School of Medicine Research Reveals Alarming Health and Resource Burden of Sleep Apnea Among U.S. Active-Duty Military
With more than 1 in 10 Americans suffering from obstructive sleep apnea putting them at increased risk of heart problems and other health ills, a new study conducted by the University of Maryland School of Medicine (UMSOM) carefully analyzed the toll that this sleep disorder takes on U.S. active-duty military members, and their analysis was alarming: They found that soldiers with sleep apnea who are serving on the front lines are more than four times more likely to experience post traumatic stress disorder and three times more likely to suffer a traumatic brain injury compared to those who don’t have the condition.

Thursday, November 21, 2024
UM School of Medicine Researchers Link Snoring to Behavioral Problems in Adolescents without Declines in Cognition
Adolescents who snore frequently were more likely to exhibit behavior problems such as inattention, rule-breaking, and aggression, but they do not have any decline in their cognitive abilities, according to a new study conducted by researchers at the University of Maryland School of Medicine (UMSOM). This is the largest study to date tracking snoring in children from elementary school through their mid-teen years and it provides an important update to parents struggling with what medical measures to take to help manage snoring in their children.
Friday, July 29, 2022
Children Who Lack Sleep May Experience Detrimental Impact on Brain and Cognitive Development That Persists Over Time, UM School of Medicine Study Finds
Elementary school-age children who get less than nine hours of sleep per night have significant differences in certain brain regions responsible for memory, intelligence, and well-being compared to those who get the recommended 9-12 hours of sleep per night, according to a new study led by University of Maryland School of Medicine (UMSOM) researchers. Such differences correlated with greater mental health problems like depression, anxiety, and impulsive behaviors in those who lacked sleep. Inadequate sleep was also linked to cognitive difficulties with memory, problem solving and decision making. The findings were published today in the journal Lancet Child & Adolescent Health.

Thursday, January 16, 2020
University of Maryland School of Medicine Research Shows That Older Patients With Untreated Sleep Apnea Need Greater Medical Care
Obstructive sleep apnea (OSA) is a common and costly medical condition leading to a wide range of health risks such as cardiovascular disease, stroke, depression, diabetes and even premature death. Researchers at the University of Maryland School of Medicine (UMSOM) found that the medical costs are substantially higher among older adults who go untreated for the disorder.

Thursday, September 28, 2017
University of Maryland School of Medicine Researchers Identify Intriguing Links Between Sleep, Cognition and Schizophrenia
More than 3.2 million Americans suffer from schizophrenia; about 100,000 people are newly diagnosed every year. The disease includes a wide range of symptoms including visual and auditory hallucinations, cognitive problems and motivational issues.
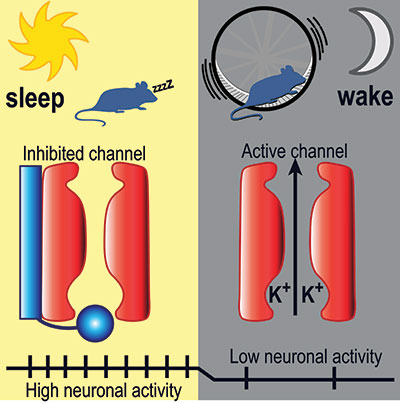
Thursday, April 14, 2016
UM SOM Research Illuminates Key Aspects of How We Fall Asleep and Wake Up
Falling asleep and waking up are key transitions in everyone’s day. Millions of people have trouble with these transitions – they find it hard to fall asleep or stay asleep at night, and hard to stay awake during the day. Despite decades of research, how these transitions work – the neurobiological mechanics of our circadian rhythm – has remained largely a mystery to brain scientists.
