December 06, 2016
Findings by University of Maryland School of Medicine Researchers Could Lead to Effective Human Vaccine for Middle East Respiratory Syndrome
In a new study, University of Maryland School of Medicine (UM SOM) researchers have modified a rabies virus, so that it has a protein from the MERS virus; this altered virus works as a 2-for-1 vaccine that protects mice against both Middle East Respiratory Syndrome (MERS) and rabies.
Because it uses an already-tested vaccine for rabies, the innovative combination could speed development of a MERS vaccine for humans. Currently no vaccine exists for this new and highly fatal virus. The study, published in the latest issue of the Journal of Virology, found that the vaccine protected mice from infection with MERS.
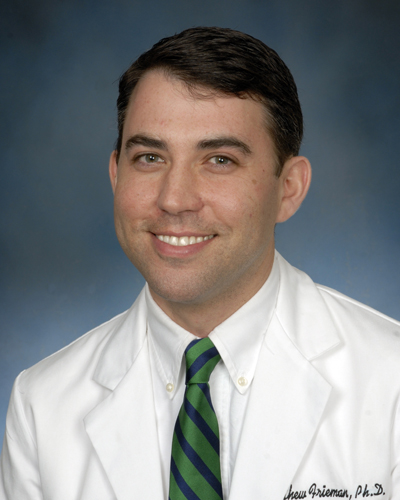
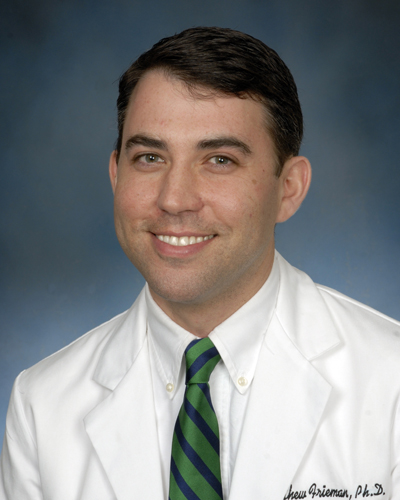
“This is the first time anyone has used this strategy to create a MERS vaccine,” said the lead researcher on the study, Matthew B. Frieman, PhD, an Associate Professor of Microbiology and Immunology at UM SOM. “This could give us a powerful mechanism to fight the virus.”
MERS has killed more than 630 people since it was first discovered four years ago in Saudi Arabia. It has infected more than 1,800, meaning that about a third of those who are infected die – a very high fatality rate for an infectious disease. It appears that the disease spreads to humans from camels, who may themselves been infected by bats. Research has shown that MERS is similar to Severe acute respiratory syndrome (SARS), which emerged in 2003 and resulted in more than 8,000 infections, killing 10 percent of patients. Both diseases, which are caused by Coronaviruses, cause serious respiratory problems.
Through genetic engineering, Dr. Frieman and his colleagues produced a modified rabies virus that expresses a protein from the surface of the MERS virus, known as a spike protein, on the surface of the rabies virus. He describes the MERS protein as a looking like a “lollypop sticking out a tennis ball.” Through an existing, FDA-approved process, scientists then treated the modified virus chemically, inactivating it so that it cannot replicate. This inactivated virus is itself the vaccine, which triggers an immune response but poses no danger to the recipient.
Because it included the MERS spike protein, the dual compound also triggered an immune response to MERS. In tests on mice, the MERS-rabies vaccine protected against both diseases. The double vaccine could prove useful not only in humans, but in camels, which are the reservoir of the disease. About 95 percent of camels in the Middle East are infected with MERS when they are young; because their immune system reacts differently from humans’, it gives them the sniffles rather than kills them. But if they were vaccinated against MERS – many of them already receive the rabies vaccine – they would not be able to spread the disease to humans. Dr. Frieman is now planning to begin testing the approach in camels.
In another recent paper, also published in the latest issue of the Journal of Virology, Dr. Frieman examined how the body responds to MERS. He examined a range of immune cells, to see which play the largest role in the body’s response to the virus. He examined three types of immune cell in particular: CD8 T cells, CD4 T cells, and macrophages. It appears that macrophages play a much larger role than the other two in protecting the body, at least in a mouse model of disease. With this knowledge, researchers will now try to understand how macrophages accomplish this. By unraveling this, they could come up with better strategies to fight MERS.
“Prof. Frieman’s work is a fantastic example of the crucial role of translational research,” said UM SOM Dean E. Albert Reece, MD, PhD, MBA, who is also the vice president for Medical Affairs, University of Maryland, and the John Z. and Akiko K. Bowers Distinguished Professor. “These studies could provide the foundation on which we one day develop cures for the worrying emerging disease that threatens not only people in other countries, but people here in the U.S.”
About the University of Maryland School of Medicine
The University of Maryland School of Medicine was chartered in 1807 and is the first public medical school in the United States and continues today as an innovative leader in accelerating innovation and discovery in medicine. The School of Medicine is the founding school of the University of Maryland and is an integral part of the 11-campus University System of Maryland. Located on the University of Maryland’s Baltimore campus, the School of Medicine works closely with the University of Maryland Medical Center and Medical System to provide a research-intensive, academic and clinically based education. With 43 academic departments, centers and institutes and a faculty of more than 3,000 physicians and research scientists plus more than $400 million in extramural funding, the School is regarded as one of the leading biomedical research institutions in the U.S. with top-tier faculty and programs in cancer, brain science, surgery and transplantation, trauma and emergency medicine, vaccine development and human genomics, among other centers of excellence. The School is not only concerned with the health of the citizens of Maryland and the nation, but also has a global presence, with research and treatment facilities in more than 35 countries around the world.
Contact
Office of Public Affairs
655 West Baltimore Street
Bressler Research Building 14-002
Baltimore, Maryland 21201-1559
Contact Media Relations
(410) 706-5260
Related stories

Friday, October 07, 2022
Other SARS-CoV-2 Proteins are Important for Disease Severity, Aside from the Spike
University of Maryland School of Medicine researchers have identified how multiple genes of SARS-CoV-2 affect disease severity, which could lead to new ways in how we develop future vaccines or develop newer treatments. The genes control the immune system of the host, contributing to how fiercely the body responds to a COVID-19 infection.

Wednesday, February 16, 2022
Study Shows New Drug Combination More Effective Against SARS-CoV-2
Researchers at the University of Maryland School of Medicine (UMSOM) and University of Pennsylvania Perelman School of Medicine have identified a powerful combination of antivirals to treat COVID-19. The researchers showed that combining the experimental drug brequinar with either of the two drugs already approved by the U.S. Food and Drug Administration for emergency use, remdesivir or molnupiravir, inhibited growth of the SARS-CoV-2 virus in human lung cells and in mice. Their findings suggest that these drugs are more potent when used in combination than individually.

Tuesday, August 24, 2021
Three UMSOM Faculty Members Recognized as 2021 Maryland Daily Record Health Care Heroes
The Maryland Daily Record has honored three leading faculty members at the University of Maryland School of Medicine (UMSOM) with its 2021 Health Care Heroes Awards. The award recognizes those who have provided exceptional service and made significant impacts on the quality of health care in the State of Maryland this year. An outside panel of health care experts selected the winners.

Friday, February 05, 2021
UM School of Medicine Researchers Demonstrate Strong Immune Response for New COVID-19 Vaccine in Pre-Clinical Tests
Researchers at the University of Maryland School of Medicine (UMSOM) have found promising results in pre-clinical studies for a new experimental vaccine against COVID-19 made by Novavax. The vaccine was found to generate a robust immune response in animals exposed to the vaccine with strong data indicating safety and efficacy, according to the study published recently in the journal Nature Communications. The results have been used to begin testing the vaccine in human trials in the U.S. with a Phase 3 trial that recently launched at the UMSOM’s Center for Vaccine Development and Global Health.

Tuesday, June 16, 2020
UM School of Medicine Researchers Receive Federal Funding to Rapidly Test New Treatments for COVID-19
Researchers at the University of Maryland School of Medicine (UMSOM) will be partnering on an agreement funded by the federal government’s Defense Advanced Research Projects Agency (DARPA) to rapidly test hundreds of drugs, approved and marketed for other conditions, to see whether any can be repurposed to prevent or treat COVID-19. The compounds will be tested in studies using state-of-the-art technologies in the laboratory of coronavirus researcher Matthew Frieman, PhD., Associate Professor of Microbiology and Immunology at the University of Maryland School of Medicine. UMSOM will receive up to $3.6 million over the next year to fund this effort.
Monday, June 15, 2020
UM School of Medicine Researchers Help Identify Potent Antibody Cocktail with Potential to Treat COVID-19
Researchers at the University of Maryland School of Medicine (UMSOM) evaluated several human antibodies to determine the most potent combination to be mixed in a cocktail and used as a promising anti-viral therapy against the virus that causes COVID-19. Their research, conducted in collaboration with scientists at Regeneron Pharmaceuticals, was published today in the journal Science. The study demonstrates the rapid process of isolating, testing and mass-producing antibody therapies against any infectious disease by using both genetically engineered mice and plasma from recovered COVID-19 patients.

Friday, October 18, 2019
Diabetes Worsens Respiratory Illness Due to Abnormal Immune Response, UM School of Medicine Study Finds
Since the Middle East respiratory syndrome coronavirus (MERS-CoV) first emerged in Saudi Arabia in 2012, there have been more than 2,400 confirmed cases of the infection, resulting in greater than 800 deaths – an alarming fatality rate of 35 percent. For this reason, researchers have been eager to identify any risk factors that contribute to the development of severe or lethal disease. Current clinical evidence points to diabetes as a major risk factor in addition to other comorbidities including kidney disease, heart disease, and lung disease.
Wednesday, February 17, 2016
New Study By UM SOM Researchers Finds Promising Results for MERS Treatment
In a new study, University of Maryland School of Medicine researchers have had promising results with a new treatment for Middle East Respiratory Syndrome (MERS). The study, published today in the journal Science Translational Medicine, found a new treatment that protected mice from MERS infection.
