Overview
Overview
The Renaissance Curriculum at the University of Maryland School of Medicine (UMSOM) was implemented in August 2020. The 150-week curriculum is designed to be completed in 4 academic years, though students may delay completion to participate in research, acquire additional academic degrees, or participate in programs to obtain specialty choices.
The curriculum's aim is to prepare our students to be successful residents within the framework of the Physician Competency Reference Set, which serves as the overall program goals. In addition, the curriculum is designed to prepare our students to achieve the mission statement of the Renaissance Curriculum: to be life-long learners who are clinically excellent and possess humanism, professionalism, scholarship, leadership, critical thinking, and attention to social justice and diversity.
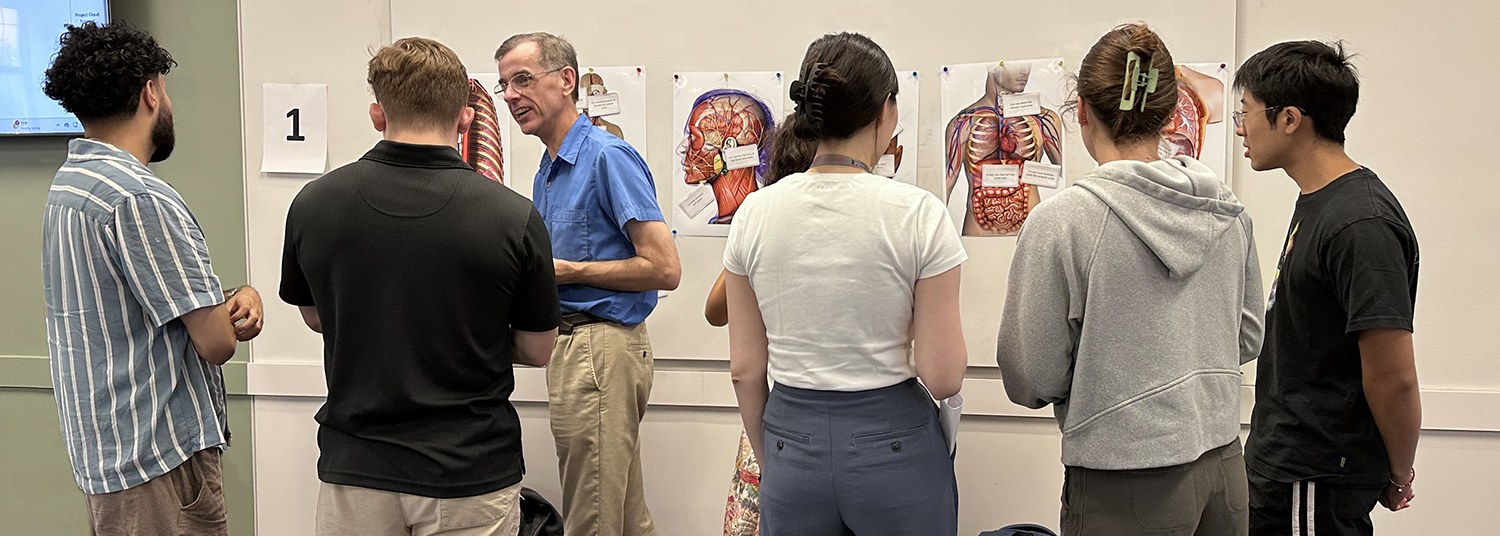
The preclerkship phase of the curriculum is an integrated, systems-based curriculum, that teaches normal and abnormal processes at the same time. Earlier interactions with patients allow students to connect and link relevant scientific material to clinical conditions. The pedagogical approach in this phase combines lectures, active-learning small-group sessions, laboratory sessions, and patient experiences with attention to collaborative learning strategies. In addition, the preclerkship phase of the Renaissance Curriculum includes a longitudinal course, Practice of Medicine. where students learn about the doctor-patient relationship and the psychosocial aspects of patients, organized medicine, and society to enable them to optimally treat a diverse group of patients.
The clinical phase provides students a series of required and elective experiences to allow them participation in a broad range of medical specialties and settings, as well as the opportunity for focused areas of clinical activity as they prepare for their career choices. The Practice of Medicine course continues in the clinical phase with particular emphasis on simulation, ultrasound, bedside teaching, and culminating with specialty specific-residency preparation and a look back into the biomedical sciences and their integration into clinical medicine.
Program and Learning Objectives
The medical education program objectives (MEPOs) were developed by the Curriculum Coordinating Committee (CCC) with input from the Office of Medical Education and Office of Student Affairs. They were reviewed and approved by the CCC in 2022. All objectives are stated in terms of the AAMC Physician Competency Reference Set (PCRS).
Outcome measures are linked to program objectives by the leaders of each course and clerkship. The medical school ensures that the outcome measures selected are appropriate through review by the Preclerkship Committee (PCC) for preclerkship courses and by the Clinical Years Committee (CYC) for clinical courses with ultimate approval by the CCC. The Curriculum Review Committee (CRC) formally reviews all required courses and clerkships on a rolling basis with periodic reviews of each phase of the curriculum and of the entire curriculum. This continuous quality improvement initiative provides course-level feedback on areas of improvement while also assuring appropriate integration between courses and phases of the curriculum.
The faculty, working through the CCC, PCC, and CYC, has framed all course and clerkship goals and objectives within the PCRS taxonomy. Both preclerkship and clinical years' goals and objectives are ultimately driven and linked to the main University of Maryland School of Medicine educational program objectives. The individual course/clerkship directors formulate goals and objectives for each educational program unit with the input of departmental faculty and leadership. These goals and objectives are then reviewed and approved by the CCC and its subcommittees. In this review process, the faculty ensures that the learning objectives of individual courses/clerkships meet the overarching program objectives.
Faculty members within each course and clerkship receive the program and learning objectives from the course or clerkship director, who is tasked with ensuring that those objectives are disseminated in the most effective way for that particular group of instructors.
Managing the Renaissance Curriculum
The CCC continuously monitors the effectiveness and cohesion of the entire curriculum; in addition, formal review of outcome measures and student feedback is undertaken annually. Outcome measures evaluated include the review of student performance on the National Board Examinations, shelf exams, Graduation Questionnaire, and faculty evaluation of student competency through direct observation (e.g., mini-CEXs). Other outcome measures such as match results (frequency per specialty, perceived quality of matched programs, student ability to obtain residency of choice) are tracked. Residency program directors complete a survey at the end of the graduate’s intern year to provide feedback to the School of Medicine on the graduate’s competency in achieving expected milestones. The results of this review are reported to the Medical Education Advisory Committee (MEAC) and the Dean; changes to the curriculum are proposed to address identified deficiencies.
Developing and reviewing the educational program objectives
The CCC and its two subcommittees, working closely with the Chief Academic Officer (Senior Associate Dean for Undergraduate Medical Education) and the MEAC, develop and periodically review and revise institutional objectives, ensure the use of appropriate teaching methods and evaluation, and monitor the effectiveness and quality of teaching. There is periodic review of goals and objectives, which undergo revision as the result of discussion and deliberations in both subcommittees and the CCC.
Ensuring that there is horizontal and vertical curriculum integration (i.e., that curriculum content is coordinated and integrated within and across academic years/phases)
Since the implementation of the Renaissance Curriculum, the PCC and the Medical Education Continuous Quality Improvement committee (MECQI) have monitored the successful integration of the preclerkship courses. The PCC and CYC include faculty representing continuous themes in the student education (embedded content leads), such as anatomy, radiology, genetics, health equity, nutrition, pharmacology, pathology, and infectious diseases. Many themes run vertically through the curriculum: examples include clinical concepts and skills which are omnipresent in the first two years, both in the form of Practice of Medicine 1 & 2 and in every preclerkship course in the form of lectures and small group sessions devoted to clinical significance of the concepts covered. The course/clerkship directors, the PCC, the CYC, and the CCC constantly work on better integration of content taught throughout the curriculum.
Monitoring the overall quality and outcomes of individual courses and clerkships
Both the PCC and CYC conduct ongoing course and clerkship review; this review includes, for example, review of student performance on internal examinations as well as the results from national examinations. In addition, both subcommittees regularly review the results of peer evaluation of teaching effectiveness, student evaluation data, as well as outcome measures. This data is reported to the CCC.
Additionally, the faculty of the School of Medicine complete a comprehensive review of the MD curriculum every 8 years through the CRC. The comprehensive review process includes:
- On-going annual reviews of student evaluations and other internal and external data (e.g., GQ, Y2Q, MMT) for every pre-clerkship course and required clerkship by the Curriculum Coordinating Committee (CCC), Pre-clerkship Curriculum Committee (PCC), Clinical years Committee (CYC), Longitudinal Integration of Curriculum Committee (LINCC), and senior administrative staff in the Office of Medical Education.
- Review of curricular phases (including a triennial review of each pre-clerkship course and required clerkships completed at three- year intervals and involving a broad range of MD program stakeholders (Course/Clerkship Directors, faculty, and medical students).
Monitoring the outcomes of the curriculum as a whole
- Evaluation of the curriculum as a whole occurs through review of medical education program objectives and related competencies in the final year of each phase review (Years 4 and 7) as well as during a whole curriculum review in year 8.
- Outcome monitoring includes the review of student performance on the National Board Examinations, shelf exams, Graduation Questionnaire, as well as faculty evaluation of student competency through direct observation (e.g., mini-CEXs). A significant outcome measures is the result of the NRMP match (i.e., frequency per specialty, perceived quality of matched programs, student ability to obtain residency of choice). Residency program directors complete a survey at the end of the graduate’s internship to provide feedback to the School of Medicine on the graduate’s competency in achieving expected milestones.
Program Requirements
The MD Program
The medical school curriculum consists of 8 full-time terms. The curriculum below represents the MD program only. See the dual-degree page for more information on our Masters, PhD and combined degrees.
Year 1 - FALL Term - Pre-clerkship Phase
| MEDS 510: Introduction to Medical School | 1 |
| MEDS 511: Foundations | 11 |
| MEDS 512: Blood & Host Defense | 8 |
| MEDS 517: Practice of Medicine I | 3 |
| Semester Credit Hours | 23 |
Year 1 - Spring Term - Pre-clerkship Phase
| MEDS 513: Brain & Behavior | 10 |
| MEDS 514: Digestion & Hormones | 8 |
| MEDS 517: Practice of Medicine I | 3 |
| Semester Credit Hours | 21 |
Year 2 - FALL Term - Pre-clerkship Phase
| MEDS 520: Clinical Integration of First Year | 1 |
| MEDS 521: Cardiovascular, Renal, & Pulmonary | 12 |
| MEDS 522: Skin, Bones, & Musculature | 7 |
| MEDS 527: Practice of Medicine II | 3 |
| Semester Credit Hours | 23 |
Year 2 - Spring Term - Pre-clerkship Phase
| MEDS 523: Life Cycle | 6 |
| MEDS 524: Multisystem | 2 |
| MEDS 527: Practice of Medicine II | 3 |
| NBME 520: USMLE Preparation | 6 |
| Semester Credit Hours | 17 |
Year 3 - Fall Term - Clerkship Phase
| MEDC 530: Core Medicine | 8 |
| GSUR 530: Core Surgery | 8 |
| EMER 530: Emergency Medicine | 4 |
| FAPH 530: Family Medicine | 4 |
| MEDS 537: Practice of Medicine III | 1 |
| Semester Credit Hours | 25 |
Year 3 - Spring Term - Clerkship Phase
| NEUR 530: Neurology | 4 |
| OBST 530: Obstetrics & Gynecology | 6 |
| PEDI 530: Pediatrics | 6 |
| PSYH 530: Psychiatry | 4 |
| Elective - 1 | 4 |
| MEDS 537: Practice of Medicine III | 1 |
| Semester Credit Hours | 25 |
Year 4 - Fall Term - Clinical Phase
| Sub-Internship - 1 | 6 |
| Electives - 3 (4 credit each) | 12 |
| NBME 540: Step 2 CK | 6 |
| Semester Credit Hours | 24 |
Year 4 - Spring Term - Clinical Phase
| Sub-Internship - 1 | 6 |
| Electives - 2 (4 credit each) | 8 |
| MEDS 547: Transition to Residency | 4 |
| FRCT 520: Scholary Project | 6 |
| OSCE 540: OSCE | 2 |
| Semester Credit Hours | 26 |
Contact OME
| Pre-Clerkship Curriculum | Clinincal Curriculum | Service Learning | Evaluation & Assessment |
|---|---|---|---|
| Devang Patel, MD | Philip Dittmar, MD | Norman Retener, MD | Connie Lecap, DO |