January 08, 2026 | Deborah Kotz

About one in nine adults suffer from chronic insomnia and its residual effects like drowsiness, cognitive issues, and irritability as well as increased health risks like diabetes and heart risks if left untreated. While many treatments are available, the challenge lies in determining how well a medication or other sleep aid works in individual patients.
Now a new study from the University of Maryland School of Medicine has found using real-time smartphone-based assessments can help to determine the effectiveness of sleep medications by detecting improvements in daytime insomnia symptoms including thinking, fatigue, and mood. Following a two-week course of treatment, this smartphone-based assessment approach detected treatment effects more powerfully than did traditional methods like recall questionnaires.
Results were published in JAMA Network Open.
 The clinical trial involved 40 older adults ages 60 to 85 with chronic insomnia who were randomly assigned to take the sleep medication suvorexant or a placebo for 16 nights. Both groups used a smartphone app to record their daytime insomnia symptoms in real-time, four times per day throughout the study. Participants also completed traditional questionnaires assessing their sleep patterns and daytime symptoms both before and after treatment.
The clinical trial involved 40 older adults ages 60 to 85 with chronic insomnia who were randomly assigned to take the sleep medication suvorexant or a placebo for 16 nights. Both groups used a smartphone app to record their daytime insomnia symptoms in real-time, four times per day throughout the study. Participants also completed traditional questionnaires assessing their sleep patterns and daytime symptoms both before and after treatment.
Key Findings
- Traditional questionnaires detected an overall improvement in insomnia severity between the treatment and placebo groups, but detected no significant differences in daytime symptoms.
- The smartphone-based assessment approach, called ecological momentary assessment (EMA), revealed subtle and important differences between the two groups: Compared to a placebo, suvorexant increased fatigue in the morning, but reduced fatigue in the afternoon and evening. Likewise, alert cognition was lower early in the day in the suvorexant group but normalized as the day progressed.
- Participants who took suvorexant reported numerically worse moods at all 4 times of day compared to those who took a placebo, although differences were not statistically significant.
- Participants found the smartphone assessment was easy to use, with a completion rate of 93.3% across all surveys, demonstrating feasibility and strong engagement.
“Daytime symptoms such as fatigue, cognitive impairment, and mood disturbances are core features of insomnia,” said study corresponding author Emerson M. Wickwire, PhD, faculty member at the University of Maryland School of Medicine and section chief of sleep medicine at the University of Maryland Medical Center. “Improving sleep is not enough. We need to determine how well treatments improve daytime functioning, which patients report matters most. In this study we found that retrospective questionnaires failed to detect subtle treatment-related changes that were detected via the smartphone assessment.”
Implications for Patients and Doctors
 This is the first randomized controlled trial to incorporate a smartphone EMA as an outcome measure in a sleep-focused clinical trial. It was able to detect clear treatment effects at various times of the day and was found to be easy to use and sustainable. Leveraging wearables and smartphones for real-time, multimethod assessment should be considered in future studies that evaluate treatment for insomnia as well as other sleep disorders including obstructive sleep apnea and excessive sleepiness that leads to prolonged sleep.
This is the first randomized controlled trial to incorporate a smartphone EMA as an outcome measure in a sleep-focused clinical trial. It was able to detect clear treatment effects at various times of the day and was found to be easy to use and sustainable. Leveraging wearables and smartphones for real-time, multimethod assessment should be considered in future studies that evaluate treatment for insomnia as well as other sleep disorders including obstructive sleep apnea and excessive sleepiness that leads to prolonged sleep.
“These findings address a critical gap in sleep disorders clinical care and research,” said Dr. Wickwire. “When viewed as a complement to traditional approaches, EMA offers a sensitive and patient-centered way to measure treatment effects throughout the day, in real-time. Such approaches could transform how we evaluate sleep treatments, personalize sleep medicine care, and ultimately improve outcomes for the millions of Americans with sleep disorders.”
Shuo Chen, PhD, Professor of Epidemiology & Public Health at UMSOM, Avelino Verceles, MD, MS, Professor of Medicine at UMSOM, and University of Maryland graduate student Jingsong Zhou, MS were co-authors on this study. Funding for this study was supported in part by a research grant from the Investigator-Initiated Studies Program of Merck Sharp & Dohme LLC, a subsidiary of Merck & Co, Inc.
“This research underscores the potential for innovative digital tools to be used in conducting comparative effectiveness studies,” said UMSOM Dean Mark T. Gladwin, MD, who is the Vice President for Medical Affairs, University of Maryland, Baltimore (UMB), and the John Z. and Akiko K. Bowers Distinguished Professor and Dean at UMSOM. "Smartphone-based assessments can provide real-time insights that help improve patient outcomes across a range of common conditions.”
Contact
Deborah Kotz
dkotz@som.umaryland.edu
Related stories

Thursday, November 21, 2024
UM School of Medicine Researchers Link Snoring to Behavioral Problems in Adolescents without Declines in Cognition
Adolescents who snore frequently were more likely to exhibit behavior problems such as inattention, rule-breaking, and aggression, but they do not have any decline in their cognitive abilities, according to a new study conducted by researchers at the University of Maryland School of Medicine (UMSOM). This is the largest study to date tracking snoring in children from elementary school through their mid-teen years and it provides an important update to parents struggling with what medical measures to take to help manage snoring in their children.
Friday, July 29, 2022
Children Who Lack Sleep May Experience Detrimental Impact on Brain and Cognitive Development That Persists Over Time, UM School of Medicine Study Finds
Elementary school-age children who get less than nine hours of sleep per night have significant differences in certain brain regions responsible for memory, intelligence, and well-being compared to those who get the recommended 9-12 hours of sleep per night, according to a new study led by University of Maryland School of Medicine (UMSOM) researchers. Such differences correlated with greater mental health problems like depression, anxiety, and impulsive behaviors in those who lacked sleep. Inadequate sleep was also linked to cognitive difficulties with memory, problem solving and decision making. The findings were published today in the journal Lancet Child & Adolescent Health.

Thursday, September 28, 2017
University of Maryland School of Medicine Researchers Identify Intriguing Links Between Sleep, Cognition and Schizophrenia
More than 3.2 million Americans suffer from schizophrenia; about 100,000 people are newly diagnosed every year. The disease includes a wide range of symptoms including visual and auditory hallucinations, cognitive problems and motivational issues.
Thursday, April 14, 2016
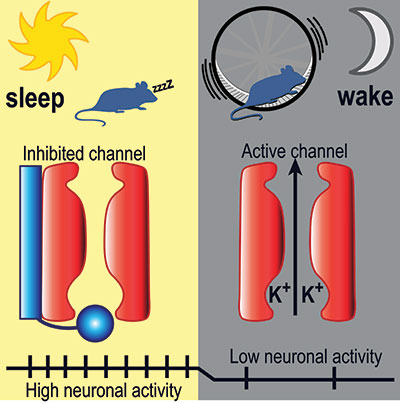
UM SOM Research Illuminates Key Aspects of How We Fall Asleep and Wake Up
Falling asleep and waking up are key transitions in everyone’s day. Millions of people have trouble with these transitions – they find it hard to fall asleep or stay asleep at night, and hard to stay awake during the day. Despite decades of research, how these transitions work – the neurobiological mechanics of our circadian rhythm – has remained largely a mystery to brain scientists.

Monday, March 14, 2016
UM SOM Sleep Experts Explore the Massive Financial Toll of Insomnia
While the benefits of a good night’s sleep can be priceless, and sleeplessness imposes significant costs on the individual and society, little is known about the financial impact of treatment for sleep-related disorders.
