March 31, 2023 | Vanessa McMains
New Finding Indicates Drug Development Targeted at Promoting Recycling Could Help Lessen Neurological Symptoms and Treat Brain Trauma
 Each year about 1.5 million people in the U.S. survive a traumatic brain injury due to a fall, car accident, or a sports injury, which can cause immediate and long-term disability.
Each year about 1.5 million people in the U.S. survive a traumatic brain injury due to a fall, car accident, or a sports injury, which can cause immediate and long-term disability.
University of Maryland School of Medicine (UMSOM) researchers wanted to better understand what happens in the brain during injury, so they conducted a study in mice to determine how different types of brain cells in mice react to severe trauma. In a new study published in the January issue of Autophagy, they found that after traumatic brain injury, the brain’s immune system cells’ internal recycling function slowed dramatically, allowing waste products to build up and interfere with recovery from injury.
The researchers also found that treating mice that had traumatic brain injury with a drug to promote cellular recycling improved the mice’s ability to recover from injury and solve a water maze, a measure of memory function in mice.
“Many drugs and potential solutions have been proposed to treat traumatic brain injury, but none have ever worked in practice,” said lead researcher Marta Lipinski, PhD, Associate Professor of Anesthesiology and Anatomy & Neurobiology at UMSOM and a member of the Shock, Trauma, and Anesthesiology Research (STAR) Center at the University of Maryland Medical Center (UMMC). “It could be that designing drugs for patients that promote this cellular recycling might reverse or prevent damage from traumatic brain injury as we saw in our animal studies. We are continuing to learn more about the molecular and cell biology mechanisms in trauma, so we can use a more guided approach for developing solutions.”
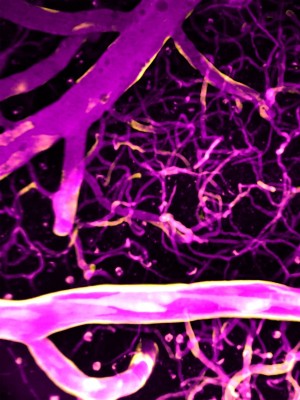
-and-autophagy-(purple)-appear-in-brain-cells-3-days-after-TBI.jpg)
The body’s cells regularly recycle their own worn-out or damaged parts that accrue through normal wear and tear, infection, or injury in a process known as autophagy. Most cells in the brain use that process for cleaning up their own waste and recycling it on a smaller scale. In a previous study, Dr. Lipinski’s group showed that traumatic brain injury reduced the ability of neurons — the cells that send electrical impulses — to recycle their own damaged parts, which then led to these neurons dying off. However, some cells in the brain can perform greater feats of recycling, such as the resident immune cells in the brain known as microglia, which can engulf, digest, and recycle entire damaged or dead cells in the tissue.
After a traumatic brain injury, white blood cells—normally excluded by the blood-brain barrier — can also get into the brain and work alongside the microglia cells to eat and remove damaged cells. For this new study, Dr. Lipinski’s team focused on the immune cells — microglia and white blood cells — in the brain after traumatic brain injury and found that, like the neurons, their recycling function was also suppressed.
 “Dr. Lipinski's discovery of the recycling function suppression in both neurons and immune cells demonstrates how important it is for neuroscientists to fully understand the complex system involved in a traumatic brain injury,” said Dean Mark Gladwin, MD, who is Vice President for Medical Affairs at the University of Maryland, Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor at UMSOM. “Developing effective drugs for traumatic brain injury treatment requires a deeper understanding of these cell-to-cell interactions and what impact each cell type has on the brain’s ecosystem.”
“Dr. Lipinski's discovery of the recycling function suppression in both neurons and immune cells demonstrates how important it is for neuroscientists to fully understand the complex system involved in a traumatic brain injury,” said Dean Mark Gladwin, MD, who is Vice President for Medical Affairs at the University of Maryland, Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor at UMSOM. “Developing effective drugs for traumatic brain injury treatment requires a deeper understanding of these cell-to-cell interactions and what impact each cell type has on the brain’s ecosystem.”
To demonstrate the full impact of the recycling process on traumatic brain injury and recovery, Dr. Lipinski and her team blocked one of the essential proteins needed to carry out the immune cell’s recycling function in the brains of mice with a brain injury. These mice experienced an even greater suppression of their cell recycling processes, resulting in more inflammation in their brain. They even performed worse, as measured by their ability to solve the water maze, than the mice with only brain injury. These findings suggested that the recycling function of the immune cells in the brain is essential for recovery after brain trauma. Conversely, boosting it may possibly lessen the impact of the trauma.
To test that, the researchers used a drug, rapamycin (normally used as a cancer drug or to prevent organ rejection), to promote cellular recycling in the brains of mice who had traumatic brain injury. The researchers found that with the treatment, the mice had lower levels of inflammation in the brain and these mice did better in navigating the water maze.
“The drug we used in our study blocks a set of proteins that are important for regenerating the body’s cells, so it cannot be used for extended time periods,” said Dr. Lipinski. “We need to continue this line of research to identify the exact mechanism of how autophagy protects against neurological damage in order to find more targeted drugs that increase this process without targeting the vital proteins needed by the brain to regenerate.”
This study was funded by grants from the National Institutes of Health’s National Institute of Neurological Disorders and Stroke (NINDS) (R01NS094527, R01NS091218, R01NS115876).
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world — with 46 academic departments, centers, institutes, and programs, and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.3 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic, and clinically based care for nearly 2 million patients each year. The School of Medicine has nearly $600 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 students, trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of over $6 billion and an economic impact of nearly $20 billion on the state and local community. The School of Medicine, which ranks as the 8th highest among public medical schools in research productivity (according to the Association of American Medical Colleges profile) is an innovator in translational medicine, with 606 active patents and 52 start-up companies. In the latest U.S. News & World Report ranking of the Best Medical Schools, published in 2021, the UM School of Medicine is ranked #9 among the 92 public medical schools in the U.S., and in the top 15 percent (#27) of all 192 public and private U.S. medical schools. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
Contact
Vanessa McMains
Director, Media & Public Affairs
University of Maryland School of Medicine
Institute of Human Virology
vmcmains@ihv.umaryland.edu
Cell: 443-875-6099
Related stories

Wednesday, April 02, 2025
Researchers Reveal Key Brain Differences to Explain Why Ritalin Helps Improve Focus in Some More Than Others
Nearly 16 million American adults have been diagnosed with attention deficit hyperactivity disorder (ADHD), but evidence suggests that more than 30 percent of them don’t respond well to stimulant medications like Ritalin and Adderall. A new clinical trial provides a surprising explanation for why this may be the case: There are individual differences in how our brains circuits are wired, including the chemical circuits responsible for memory and concentration, according to a new study co-led by the University of Maryland School of Medicine (UMSOM) and performed at the National Institutes of Health (NIH) Clinical Center.

Thursday, May 25, 2023
Longtime Anesthesiology Department Chair and Academic Leader Peter Rock, MD, MBA to Step Down as Chair, Will Return to Faculty
Peter Rock, MD, the Dr. Martin Helrich Professor and Chair of Anesthesiology at the University of Maryland School of Medicine (UMSOM), announced today that he will be stepping down from his longtime administrative role as Department Chair this summer to return to full-time faculty status.

Tuesday, April 25, 2023
Immune System Sculpts Rat Brains During Development
Researchers have established that biological sex plays a role in determining an individual’s risk of brain disorders. For example, boys are more likely to be diagnosed with behavioral conditions like autism or attention deficit disorder, whereas women are more likely to suffer from anxiety disorders, depression, or migraines. However, experts do not fully understand how sex contributes to brain development, particularly in the context of these diseases. They think, in part, it may have something to do with the differing sizes of certain brain regions.

Friday, January 06, 2023
UM School of Medicine Scientists Create First Extensive Brain Cell Data Repository
Neuroscience researchers now have access to 50 million brain cells to better understand how the brain develops and functions or changes with disease or trauma. Last month, scientists at the University of Maryland School of Medicine’s (UMSOM) Institute for Genome Sciences (IGS) unveiled a “one-stop shop” for brain cell data called the Neuroscience Multi-Omic Archive (NeMO Archive). This archive is now available to neuroscience researchers to transform their understanding of the complex workings of the brain.

Monday, November 14, 2022
Brain Area Thought to Impart Consciousness, Behaves Instead Like an Internet Router
Tucked underneath the brain’s outer, wrinkly cortex is a deeply mysterious area, known as the claustrum. This region has long been known to exchange signals with much of the cortex, which is responsible for higher reasoning and complex thought. Because of the claustrum’s extensive connections, the legendary scientist Francis Crick, PhD, of DNA-discovery fame, first postulated in 2005 that the claustrum is the seat of consciousness. In other words, the region of the brain enabling awareness of the world and ourselves.
Wednesday, July 21, 2021
University of Maryland School of Medicine Study Finds Calcium Precisely Directs Blood Flow in the Brain
University of Maryland School of Medicine and University of Vermont researchers have shown how the brain communicates to blood vessels when in need of energy, and how these blood vessels respond by relaxing or constricting to direct blood flow to specific brain regions.

Wednesday, September 25, 2019
Dr. Tracy Bale Elected President of the International Brain Research Organization
Tracy L. Bale, PhD, Professor of Pharmacology and Director of the Center for Epigentic Research in Child Health & Brain Development has been elected President of the International Brain Research Organization.

Monday, April 29, 2019
UMSOM’s Reading on the Brain Program Teaches Baltimore City Elementary Students About the Brain-Building Power of Reading
Acting Baltimore City Mayor Jack Young joined 4th and 5th grade students at Callaway Elementary School to help paint a mural about the brain. It was all part of Reading on the Brain, a University of Maryland School of Medicine (UMSOM) program to teach young students about the importance of reading and how reading can stimulate brain development and inspire future success. Tracy Bale, PhD, is leading the pilot program, which also emphasizes science and helps children to understand how the brain works.

Thursday, March 28, 2019
Allergic Reactions Play Role in Sexual Behavior Development in Unborn Males and Females, UMSOM Research Shows
Researchers at the University of Maryland School of Medicine and colleagues at Ohio State University have discovered that allergic reactions trigger changes in brain behavior development in unborn males and females. This latest brain development discovery will ultimately help researchers better understand how neurological conditions can differ between men and women.

Friday, March 01, 2019
UMSOM Researchers Discover Clues to Brain Differences Between Males and Females
Researchers at the University of Maryland School of Medicine have discovered a mechanism for how androgens -- male sex steroids -- sculpt brain development. The research, conducted by Margaret M. McCarthy, Ph.D., Professor of Pharmacology and Chair of the Department of Pharmacology, could ultimately help researchers understand behavioral development differences between males and females.

Thursday, December 07, 2017
University of Maryland School of Medicine Scientists Identify the First Brain Cells to Respond to Sound
Some expectant parents play classical music for their unborn babies, hoping to boost their children’s cognitive capacity. While some research supports a link between prenatal sound exposure and improved brain function, scientists had not identified any structures responsible for this link in the developing brain.

