February 17, 2023 | Vanessa McMains
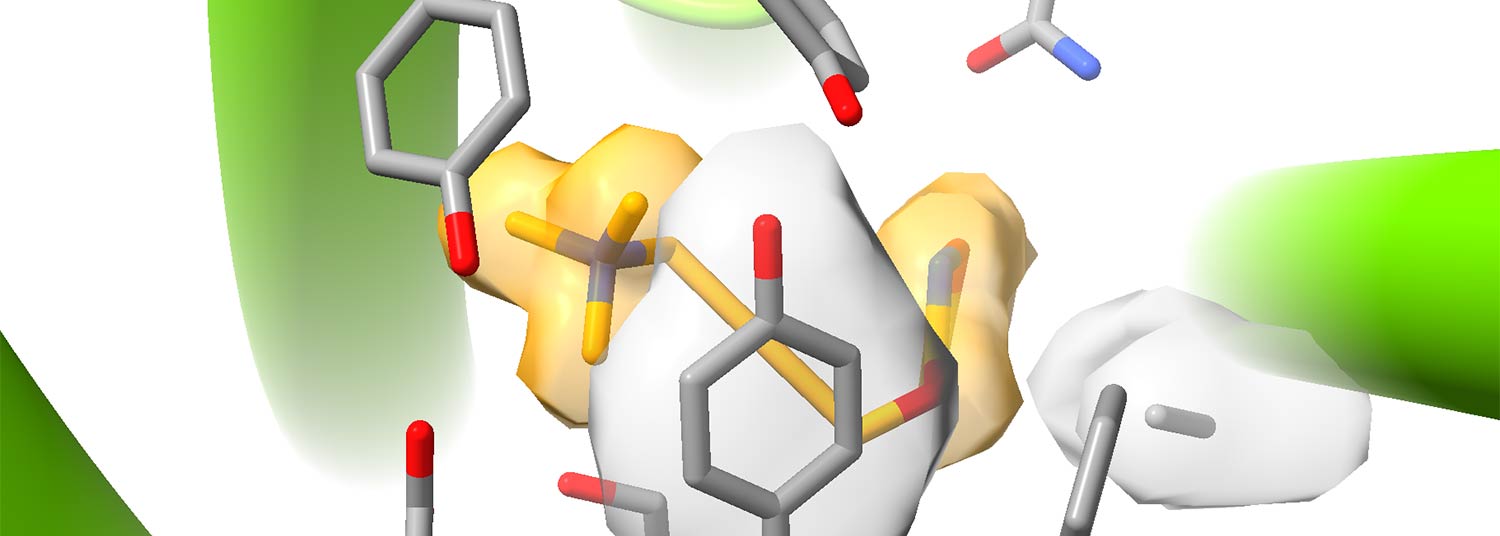
Structure of a DREADD designer receptor (green/yellow/white) with a designer drug bound (gray stick figure).
Newer Technology Will Allow Better Understanding of the Brain to Ultimately Develop Innovative Treatments
 In order to more fully understand how diseases arise in the brain, scientists must unravel the intricate way neurons relay messages (either chemical or electrical) along a complex web of nerve cells. One way is by using a tool called DREADDs, which stands for Designer Receptors Activated by Designer Drugs.
In order to more fully understand how diseases arise in the brain, scientists must unravel the intricate way neurons relay messages (either chemical or electrical) along a complex web of nerve cells. One way is by using a tool called DREADDs, which stands for Designer Receptors Activated by Designer Drugs.
When introduced to a nerve cell or neuron, DREADDs acts like a specialized lock that only works when a key — in the form of a synthetic designer drug — fits into that lock. DREADDs can enable researchers to turn specific cell functions on or off to examine groups of neurons in circuits more precisely. (see Animations)
Now, a University of Maryland School of Medicine researcher and his colleagues at the University of North Carolina Chapel Hill (UNC) have unveiled the structure of these DREADDs that will pave the way for creating the next generation of these tools. This step ultimately will bring them closer to an elusive goal — understanding the underpinnings of brain disorders, such as schizophrenia, substance abuse, epilepsy, and Alzheimer’s, in order to develop more effective drugs to treat them.
The research team published their findings in a recent issue of Nature.
“These findings provide atomic clarity into the nature of DREADD receptors bound to their drugs, resulting from the culmination of all these technologies converging at the right place and right time,” said study author Jonathan Fay, PhD, Assistant Professor of Biochemistry and Molecular Biology at UMSOM. “This knowledge will allow this tool to be further refined and optimized. We were previously limited in how to upgrade their designs because we didn’t fully understand how they worked at the structural level.”
Hundreds of labs around the world now use the DREADD tool, which was developed at UNC. Scientists there designed these receptor proteins to react only to uniquely designed drugs that are pharmacologically inert because they only bind to the DREADD protein receptor.
For this new study, researchers used a newer imaging technology, known as cryogenic electron microscopy, to determine the molecular structure of DREADD receptors with the drugs. This process flash-freezes the DREADDs in a way that does not form traditional ice crystals, but instead creates a sort of slurry that allows some movement in the molecules. This technique allowed researchers to determine the DREADD’s structure when other older molecular imaging methods failed. The researchers observed inhibitory (turning off cell functions) or stimulatory (turning on cell functions) DREADD receptors bound to each of two different designer drugs.
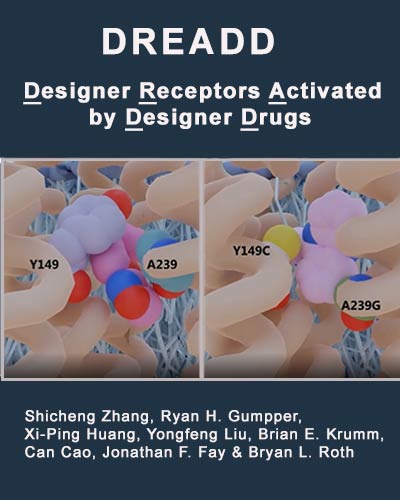
The researchers also compared the structure of the natural brain receptor from which DREADDs originated to see how it differed from DREADDs. The original brain receptor, found in the cell membrane of neurons, traditionally binds to a molecule involved in learning and memory. By changing two of the natural receptor’s building blocks, the engineered DREADD receptor binds better to its own laboratory-designed drugs rather than to the original memory molecule—a process they visualized through their experiments.
“With this imaging technique, we could see that the genetic changes in the DREADDs opened up the space where the memory molecule normally binds, allowing the new designer drugs to slip in. We could see that shape of the space changed as well, contributing to why the new drugs fit better,” said Dr. Fay.
The class of receptors from which DREADDs originated are often the intended targets of many therapeutics. However, various drugs bind to several kinds of receptors or activate others in unintended ways. The result might be a beneficial effect, but also can result in side effects.
 “Because of the precise way in which these designer drugs in DREADDs bind so specifically, it is likely possible that researchers will one day eventually develop targeted therapies for many of these other similar receptors without the cross-reactivity and unpleasant side effects,” said UMSOM Dean Mark T. Gladwin, MD, Vice President for Medical Affairs, University of Maryland, Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor.
“Because of the precise way in which these designer drugs in DREADDs bind so specifically, it is likely possible that researchers will one day eventually develop targeted therapies for many of these other similar receptors without the cross-reactivity and unpleasant side effects,” said UMSOM Dean Mark T. Gladwin, MD, Vice President for Medical Affairs, University of Maryland, Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor.
Although the microscopy-related part of this study occurred at UNC, UMSOM also has high-tech structural biology capabilities in their Center for Biomolecular Therapeutics (CBT), where researchers determine the structures of the human body’s proteins to better develop new drugs to treat a variety of diseases. Dr. Fay plans to use CBT’s facilities to analyze the structure of other brain receptors, as well as to continue his collaboration with UNC on potential DREADD 2.0 versions.
A major focus of UMSOM’s research, as evidenced by the launch of the University of Maryland-Medicine Institute for Neuroscience Discovery (UM-MIND) in late 2022 includes neuroscience and brain-related diseases. Dr. Fay’s work directly contributes towards these institutional priorities.
This research study was funded by a National Institutes of Health - National Institute of Diabetes and Digestive and Kidney Diseases grant (U24DK116194).
Animations
 |
 |
| Three DREADD receptors (cream; left panels duplicated in each video) with three different designer drugs bound. | |
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world — with 46 academic departments, centers, institutes, and programs, and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.3 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic, and clinically based care for nearly 2 million patients each year. The School of Medicine has nearly $600 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 students, trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of over $6 billion and an economic impact of nearly $20 billion on the state and local community. The School of Medicine, which ranks as the 8th highest among public medical schools in research productivity (according to the Association of American Medical Colleges profile) is an innovator in translational medicine, with 606 active patents and 52 start-up companies. In the latest U.S. News & World Report ranking of the Best Medical Schools, published in 2021, the UM School of Medicine is ranked #9 among the 92 public medical schools in the U.S., and in the top 15 percent (#27) of all 192 public and private U.S. medical schools. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
Contact
Vanessa McMains
Director, Media & Public Affairs
University of Maryland School of Medicine
Institute of Human Virology
vmcmains@ihv.umaryland.edu
Cell: 443-875-6099
Related stories

Monday, July 24, 2023
Structure of Opioid Receptors May Reveal How to Better Design Pain Relievers, Addiction Therapies
Opioids remain the most potent and effective pain relievers in medicine, but they’re also among the most addictive drugs that can halt a person’s ability to breathe during an overdose — which can be deadly. Researchers have been racing to develop safer pain reliever drugs that target a specific opioid receptor, called the kappa opioid receptor, that is only found in the central nervous system and not elsewhere in the body, like other opioid receptors. Previous research suggests that such drugs may not lead to addiction or death due to overdose, but the currently known drugs that target these kappa opioid receptors have their own set of unacceptable side effects, including depression and psychosis.
