October 07, 2022 | Vanessa McMains
University of Maryland School of Medicine researchers have identified how multiple genes of SARS-CoV-2 affect disease severity, which could lead to new ways in how we develop future vaccines or develop newer treatments. The genes control the immune system of the host, contributing to how fiercely the body responds to a COVID-19 infection.
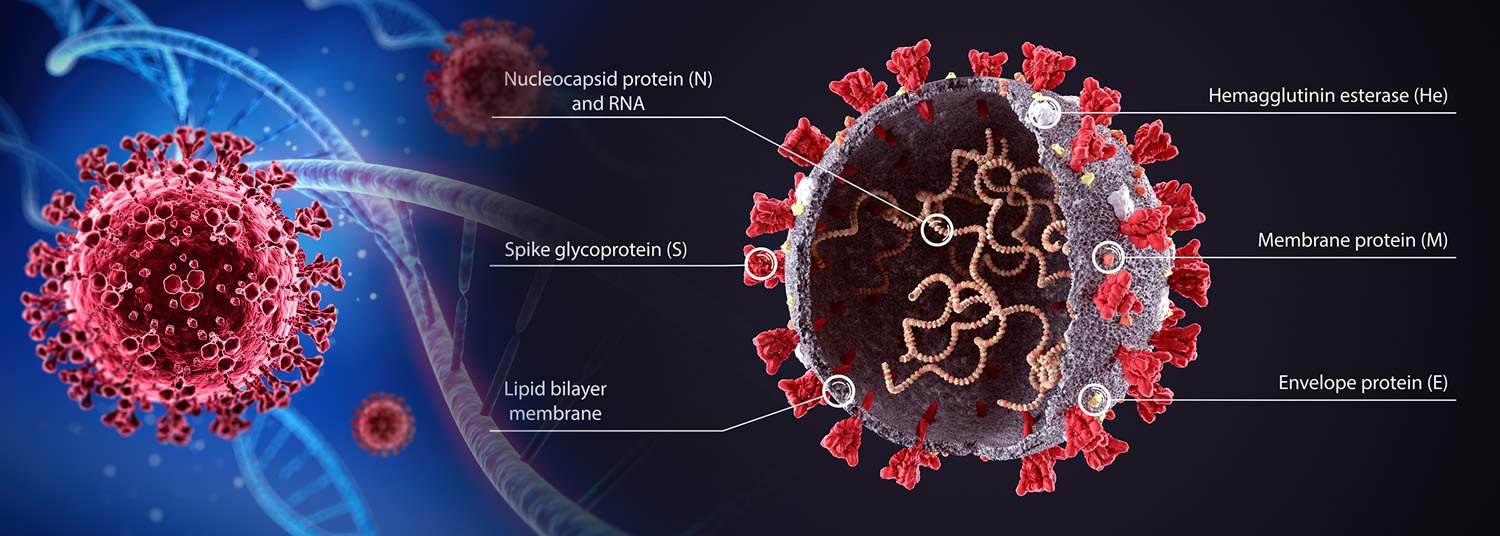
Although people typically think of the spike protein that forms the structural “crown” as the driving factor behind each new variant of COVID-19, research findings also show that mutations in these other “accessory” genes also play a role in how the disease progresses. Because of this, researchers believe these accessory proteins warrant further study as their mutations increasingly may become more significant as newer variants arise.
Their findings were published on August 30, 2022, in PNAS.
 The BA.4 variant of Omicron, which circulated earlier this year, was overtaken by the latest BA.5 variant of the virus circulating now. Both of these variants seem to evade the immune system due to mutations in the spike protein. Because of these spike mutations, the researchers say the previous vaccines are not as effective in preventing disease.
The BA.4 variant of Omicron, which circulated earlier this year, was overtaken by the latest BA.5 variant of the virus circulating now. Both of these variants seem to evade the immune system due to mutations in the spike protein. Because of these spike mutations, the researchers say the previous vaccines are not as effective in preventing disease.
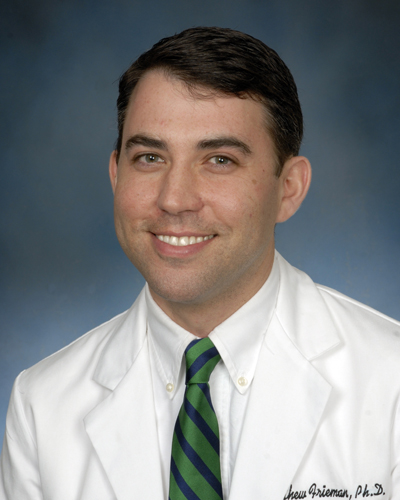
“What is interesting is that both BA.4 and BA.5 variants have the same genetic sequence for the spike protein,” said Matthew Frieman, PhD, Alicia and Yaya Foundation Professor of Viral Pathogen Research in The Department of Microbiology & Immunology at UMSOM. “This means it’s the other genes, the non-spike protein genes, that seem to affect the way the virus copies itself and causes disease. So, mutations in these other accessory genes are what has allowed variants like BA.5 to outcompete the earlier versions of the virus.”
The SARS-CoV-2 virus has three kinds of genes — those involved in making more copies of the virus, those that make the virus structure, and accessory genes that have other functions. For this new study, the researchers wanted to find out the function of the accessory genes. To do this, they recreated viruses missing each of four accessory proteins and then infected mice with these new viruses or the original virus. Next, they observed how each virus affected the mice.
Dr. Frieman’s team of researchers found that virus missing the ORF3a/b gene led to more mild infections than the original SARS-CoV-2 virus. The mice with this virus strain lost less weight and had less virus in their lungs than mice infected with the original virus. These findings indicated that the ORF3a/b gene likely plays a role in either making more copies of the virus through viral replication or blocking the immune response to the infection. Other experiments suggested ORF3a/b has an extra job in the virus by seeming to activate the body’s innate immune system, the first line of defense launched by the immune system, signaling that a foreign invader needs to be vanquished.
In contrast, the researchers found that mice infected with virus missing the ORF8 gene were sicker than mice with the original strain of SARS-CoV-2. These mice had increased inflammation in their lungs when compared with the original SARS-CoV-2 virus. The researchers said that ORF8 seems to control the immune response in the lungs.
“By inhibiting the immune response, ORF8 helps the virus to replicate more in the lungs which worsens infection. When removed, it allowed the immune system to fight back harder,” said Dr. Frieman.
Next, the researchers looked at how important the spike protein was for disease severity in each of the different variants of SARS-CoV-2. They took the original virus and swapped out the spike gene with the spike gene of either the alpha, beta, gamma, or delta variant. Then they infected cells and mice and observed how each of these viruses replicated and entered healthy cells. The virus uses the spike protein to hitchhike on the host’s ACE2 receptors found on the outside of cells lining the lungs as a way to get inside and infect cells.
 Dr. Frieman’s team found that the spike protein determines the severity of some of the variants, but not for others. The gamma variant was weaker than the other variants in its ability to replicate and infect. The researchers think that the mutations in genes outside of the ‘spike,’ particularly in the ORF8 gene, seem to play a role in making this version weaker than the others. Although the gamma variant circulated in Brazil, it did not spread further around the globe as it was overtaken by stronger variants.
Dr. Frieman’s team found that the spike protein determines the severity of some of the variants, but not for others. The gamma variant was weaker than the other variants in its ability to replicate and infect. The researchers think that the mutations in genes outside of the ‘spike,’ particularly in the ORF8 gene, seem to play a role in making this version weaker than the others. Although the gamma variant circulated in Brazil, it did not spread further around the globe as it was overtaken by stronger variants.
“While the spike mutations are important for enhancing receptor binding and entry into cells, the researchers also found that the mutations in the accessory proteins can alter clinical disease presentation,” said Mark T. Gladwin, MD, Vice President for Medical Affairs at University of Maryland, Baltimore and the John Z. and Akiko K. Bowers Distinguished Professor and Dean, UMSOM. “We need to learn more about the role of accessory protein mutations in COVID-19 infection, especially as new variants and subvariants keep emerging where these other proteins may play more of a starring role.”
The researchers plan to focus on dissecting more of ORF8’s function in future studies.
Additional UMSOM authors include Graduate Student Marisa McGrath, Postdoc Carly Dillen, PhD, Research Technician Lauren Baracco, and Postdoc Louis Taylor, PhD;other study coauthors were from the J. Craig Venter Institute.
This work was supported by grants from The Bill and Melinda Gates Foundation, the National Institute of Allergy and Infectious Diseases (R01AI137365 and R03AI146632), and the J. Craig Venter Institute.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 46 academic departments, centers, institutes, and programs, and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.3 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic, and clinically based care for nearly 2 million patients each year. The School of Medicine has nearly $600 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 students, trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of over $6 billion and an economic impact of nearly $20 billion on the state and local community. The School of Medicine, which ranks as the 8th highest among public medical schools in research productivity (according to the Association of American Medical Colleges profile) is an innovator in translational medicine, with 606 active patents and 52 start-up companies. In the latest U.S. News & World Report ranking of the Best Medical Schools, published in 2021, the UM School of Medicine is ranked #9 among the 92 public medical schools in the U.S., and in the top 15 percent (#27) of all 192 public and private U.S. medical schools. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
Contact
Vanessa McMains
Director, Media & Public Affairs
University of Maryland School of Medicine
Institute of Human Virology
vmcmains@ihv.umaryland.edu
Cell: 443-875-6099
Related stories

Wednesday, February 16, 2022
Study Shows New Drug Combination More Effective Against SARS-CoV-2
Researchers at the University of Maryland School of Medicine (UMSOM) and University of Pennsylvania Perelman School of Medicine have identified a powerful combination of antivirals to treat COVID-19. The researchers showed that combining the experimental drug brequinar with either of the two drugs already approved by the U.S. Food and Drug Administration for emergency use, remdesivir or molnupiravir, inhibited growth of the SARS-CoV-2 virus in human lung cells and in mice. Their findings suggest that these drugs are more potent when used in combination than individually.

Friday, February 05, 2021
UM School of Medicine Researchers Demonstrate Strong Immune Response for New COVID-19 Vaccine in Pre-Clinical Tests
Researchers at the University of Maryland School of Medicine (UMSOM) have found promising results in pre-clinical studies for a new experimental vaccine against COVID-19 made by Novavax. The vaccine was found to generate a robust immune response in animals exposed to the vaccine with strong data indicating safety and efficacy, according to the study published recently in the journal Nature Communications. The results have been used to begin testing the vaccine in human trials in the U.S. with a Phase 3 trial that recently launched at the UMSOM’s Center for Vaccine Development and Global Health.

Tuesday, June 16, 2020
UM School of Medicine Researchers Receive Federal Funding to Rapidly Test New Treatments for COVID-19
Researchers at the University of Maryland School of Medicine (UMSOM) will be partnering on an agreement funded by the federal government’s Defense Advanced Research Projects Agency (DARPA) to rapidly test hundreds of drugs, approved and marketed for other conditions, to see whether any can be repurposed to prevent or treat COVID-19. The compounds will be tested in studies using state-of-the-art technologies in the laboratory of coronavirus researcher Matthew Frieman, PhD., Associate Professor of Microbiology and Immunology at the University of Maryland School of Medicine. UMSOM will receive up to $3.6 million over the next year to fund this effort.
Monday, June 15, 2020
UM School of Medicine Researchers Help Identify Potent Antibody Cocktail with Potential to Treat COVID-19
Researchers at the University of Maryland School of Medicine (UMSOM) evaluated several human antibodies to determine the most potent combination to be mixed in a cocktail and used as a promising anti-viral therapy against the virus that causes COVID-19. Their research, conducted in collaboration with scientists at Regeneron Pharmaceuticals, was published today in the journal Science. The study demonstrates the rapid process of isolating, testing and mass-producing antibody therapies against any infectious disease by using both genetically engineered mice and plasma from recovered COVID-19 patients.

Friday, October 18, 2019
Diabetes Worsens Respiratory Illness Due to Abnormal Immune Response, UM School of Medicine Study Finds
Since the Middle East respiratory syndrome coronavirus (MERS-CoV) first emerged in Saudi Arabia in 2012, there have been more than 2,400 confirmed cases of the infection, resulting in greater than 800 deaths – an alarming fatality rate of 35 percent. For this reason, researchers have been eager to identify any risk factors that contribute to the development of severe or lethal disease. Current clinical evidence points to diabetes as a major risk factor in addition to other comorbidities including kidney disease, heart disease, and lung disease.
Tuesday, December 06, 2016
Researchers Combine MERS and Rabies Viruses to Create Innovative 2-For-1 Vaccine
In a new study, University of Maryland School of Medicine (UM SOM) researchers have modified a rabies virus, so that it has a protein from the MERS virus; this altered virus works as a 2-for-1 vaccine that protects mice against both Middle East Respiratory Syndrome (MERS) and rabies.
