Mission Statement
The goal of our residency education program is to cultivate an educational environment which provides the full spectrum of learning opportunities in clinical medical physics, radiation oncology, and radiobiology.
Program Overview
The University of Maryland Radiation Oncology Medical Physics Residency Program is a two-year training program.
Program Overview
 Our flexible curriculum is designed to enable residents to optimize their learning experience throughout their two years of training. It is our expectation that upon completion of the program, a resident will be an outstanding radiation oncology physicist, capable of making immediate impacts in either academic or community practice settings.
Our flexible curriculum is designed to enable residents to optimize their learning experience throughout their two years of training. It is our expectation that upon completion of the program, a resident will be an outstanding radiation oncology physicist, capable of making immediate impacts in either academic or community practice settings.
Program Directors' Welcome
On behalf of the entire faculty, we would like to welcome you to the University of Maryland Medical Physics Residency Program.
We are committed to providing you with a comprehensive clinical medical physics training experience that will supply you with all of the tools necessary for you to graduate as an accomplished medical physicist with a strong emphasis on safety, quality, innovation, and leadership. Our goal is to produce high-performing clinical medical physicists who are future leaders in our field.
The University of Maryland offers a diverse clinical experience and incorporates training with state-of-the-art technology including pencil beam scanning proton therapy, stereotactic radiation, brachytherapy, radioembolization, the unique GammaPod™ invented at the University of Maryland, and hyperthermia therapy. As a leading academic center, we also offer a rich clinical research experience along with top-notch faculty mentorship experiences.
Our faculty provide a supportive environment for learning, and our physics residency program is invested in helping you develop both as a person and as a professional. We value and respect all of our residents, faculty, and staff, and provide an open and welcoming environment where employees are respected and heard, regardless of their position or status within the department. Our department's unique and active Together We Thrive Committee has a resident member to help represent the input of our trainees.
Please take a look at the website which we hope offers an overview of some of the advantages of the training program at the University of Maryland. If you have further questions, feel free to contact us for more information. We hope you consider applying to our program so that we can show you all our residency has to offer!
Warmly,
Arun and Jochen

Arun Gopal, PhD, DABR
Associate Professor
Director of the Medical Physics Residency Program
Department of Radiation Oncology

Jochen Cammin, D.Sc.
Assistant Professor
Associate Director of the Medical Physics Residency Program
Department of Radiation Oncology
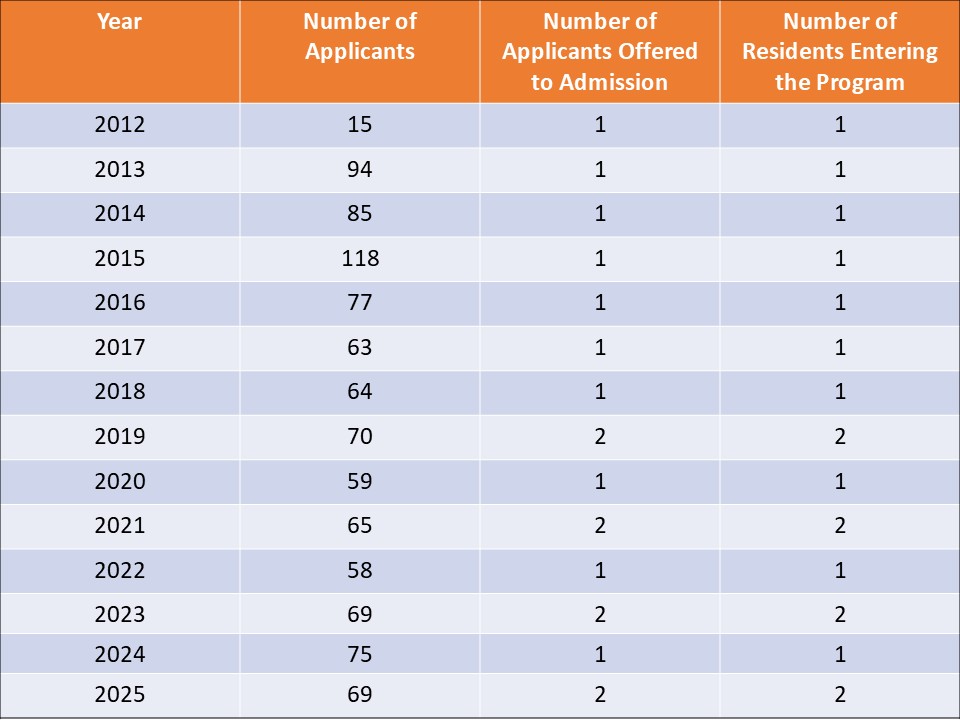
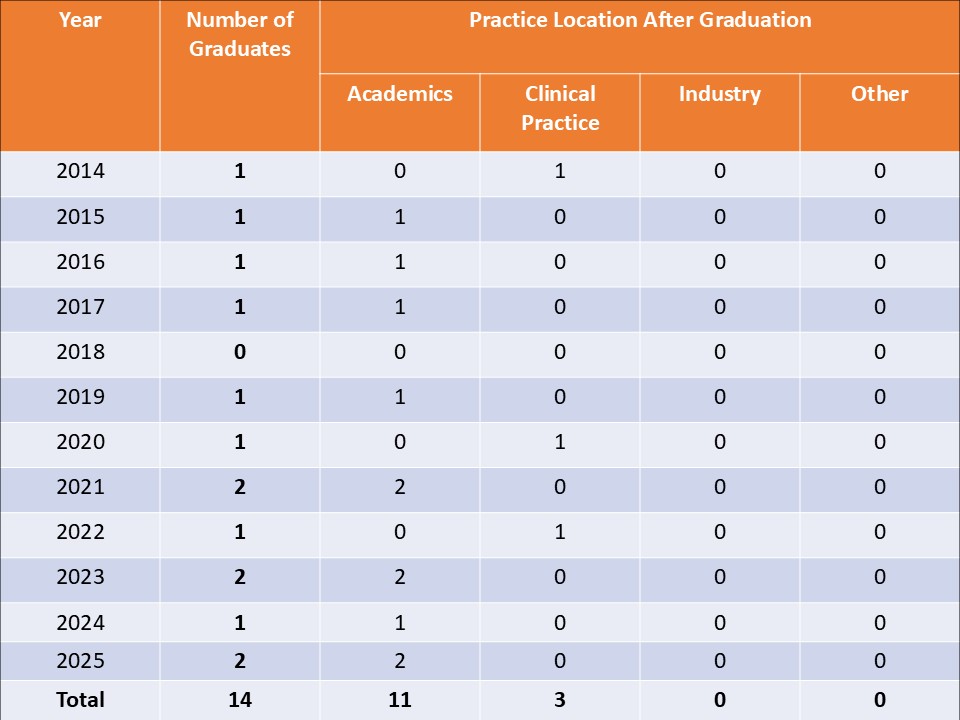
Numbers of Applicants & Graduates
CAMPEP Residency Standard 2.13 states:
"An accredited program must publicly describe the program and the achievements of its residents, preferably through a publicly-accessible website, readily accessible from the program website home page. This information must be updated no less often than annually and must include the numbers of applicants to the program, of applicants offered admission, of residents entering the program, and of graduates. Information on the subsequent positions of graduates shall also be provided, i.e., numbers in academics, clinical practice, industrial positions, etc. This information should not identify individuals."
The following tables provide such information:
Physics Residency Program Applicants
Physics Residency Program Graduates
Together We Thrive

We value all of our department’s faculty, trainees, staff, and patients. We aim to recruit and support trainees from a wide range of backgrounds and experiences, and provide an engaging, inclusive, and welcoming learning environment for all. Our residents and leaders welcome open communication and conversations. Our medical physics residents come from a variety of backgrounds, countries of birth, and, educational institutions across the world.
Members of the Department of Radiation Oncology are leaders in addressing healthcare disparities and the cancer care needs of underserved populations. Under-resourced patients represent nearly half of those enrolled in UMMC/UMGCCC clinical trials, which is three times the national average.
Our department has an active Together We Thrive Committee, which offers multiple professional trainings and seminars to employees throughout the year, and all residents are encouraged and supported to participate in Thrive Committee events.
Dr. Karl L. Prado Endowment for Radiation Oncology Trainees
Help Fund the Next Generation of Cancer Treatment Specialists

Karl L. Prado, PhD, FACR, FAAPM
1950–2018
Dr. Karl L. Prado served as a faculty member and invaluable medical physics educator to trainees and staff from 2009 to 2017 at the University of Maryland Department of Radiation Oncology. In 2019, the department renamed the Dr. Karl Prado Physics and Radiobiology Review Course to honor the memory of Dr. Karl Prado and recognize his unmatched teaching abilities.
The Dr. Prado endowment helps support our educational mission by funding trainees, medical and physics residents, fellows, radiation therapists, dosimetrists, nurses, and medical students for a number of initiatives including attendance at research conferences, educational events, training, wellness activities, and elective rotations.
Your support of the Dr. Karl L. Prado Endowment for Radiation Oncology captures your dedication to all facets of training and continuing education which enables our trainees to help save lives through their work.
Give to the Dr. Karl L. Prado Endowment for Radiation Oncology Trainees