October 31, 2025 | Jon Kelvey
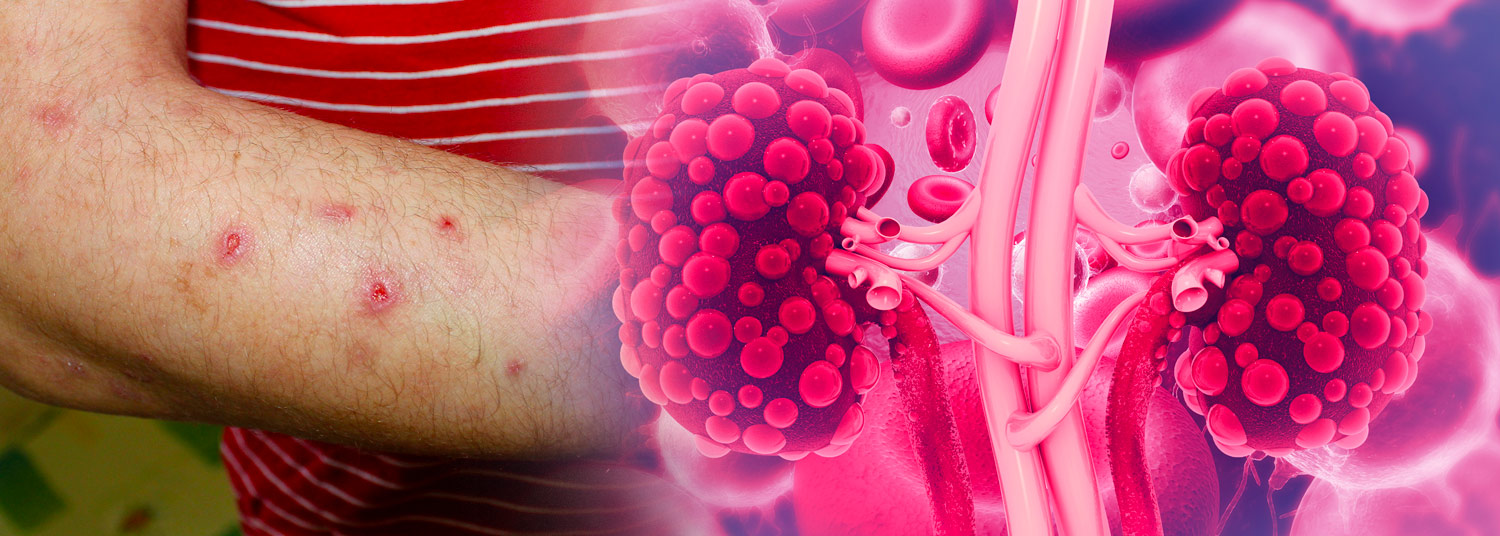
University of Maryland School of Medicine (UMSOM) researchers have uncovered new biological evidence linking the chronic skin disorder prurigo nodularis with subclinical kidney damage.
The findings, published in the Journal of the American Academy of Dermatology International, identified circulating biomarkers associated with subclinical kidney injury in prurigo nodularis patients, suggesting a role for undertreatment of the skin disease in damaging end organs and potential new approaches for assessing and treating the condition.
 Characterized by firm, intensely itchy nodules on the skin, prurigo nodularis can severely impact a patient's quality of life. Traditionally considered a condition limited to the skin, prurigo nodularis is increasingly seen as the dermatologic manifestation of systemic inflammation affecting other organs. Recent epidemiological studies, for example, found that prurigo nodularis patients had a significantly increased risk of chronic kidney disease.
Characterized by firm, intensely itchy nodules on the skin, prurigo nodularis can severely impact a patient's quality of life. Traditionally considered a condition limited to the skin, prurigo nodularis is increasingly seen as the dermatologic manifestation of systemic inflammation affecting other organs. Recent epidemiological studies, for example, found that prurigo nodularis patients had a significantly increased risk of chronic kidney disease.
Evidence of Inflammatory Biomarkers
The new findings by the UMSOM research team, led by Shawn Kwatra, MD, the Joseph W. Burnett Endowed Professor and Chair in Dermatology, identify biological mechanisms behind the association between kidney disease and prurigo nodularis, suggesting undertreatment of prurigo nodularis may result in end-organ kidney damage.
In the study, researchers identified prurigo nodularis patients with no known history of kidney or cardiac conditions, and matched them with healthy control participants. In analyzing the blood plasma of the participants, they found significantly elevated levels of inflammatory biomarkers associated with kidney injury in the plasma of the prurigo nodularis patients compared with the controls. These biomarkers include: α1-microglobulin, Collagen IV, Lipocalin-2, Tissue Inhibitor of Metalloproteinase-1 (TIMP-1), Uromodulin, and Osteoactivin. The researchers hypothesize that Osteoactivin, also known as glycoprotein non-metastatic melanoma protein B (GPNMB), may play a key role in prurigo nodularis, due to its known role in fibrotic signaling.
 “Our study reveals subclinical damage to the kidney in untreated prurigo nodularis patients," said Dr. Kwatra, who is also the Director of the Maryland Itch Center, and an internationally recognized expert on prurigo nodularis. "These elevated levels markers even in patients without existing chronic kidney disease, strongly suggest that the systemic inflammation driving prurigo nodularis is also inducing subclinical renal stress.”
“Our study reveals subclinical damage to the kidney in untreated prurigo nodularis patients," said Dr. Kwatra, who is also the Director of the Maryland Itch Center, and an internationally recognized expert on prurigo nodularis. "These elevated levels markers even in patients without existing chronic kidney disease, strongly suggest that the systemic inflammation driving prurigo nodularis is also inducing subclinical renal stress.”
Possible Inflammatory Link Between Pruritus and Kidney Disease
Conversely, Dr. Kwatra added, patients with advanced kidney disease frequently experience pruritus, suggesting a possible bidirectional relationship between kidney disease and the skin disorder. Given the limitations of the present study’s relatively small sample size and cross-sectional design, he said, further assessment of the relationship between prurigo nodularis and renal dysfunction will require further, longitudinal studies.
In the meantime, routine assessment of renal stress biomarkers in prurigo nodularis patients could provide clinicians a crucial window for early interventions to reduce the risk of irreversible kidney damage.
"The results suggest that a more comprehensive, systemic treatment approach, combining dermatological care with early lifestyle modifications and systemic treatments, may be necessary to reduce both the burden of the skin disease and its associated comorbid risks,” Dr. Kwatra said.
About the University of Maryland School of Medicine
The University of Maryland School of Medicine, established in 1807 as the first public medical school in the U.S., continues today as one of the fastest growing, top-tier biomedical research enterprises in the world. The School has nearly $500 million total research funding, 46 departments, centers, and institutes, more than 2,200 student trainees and over 3,000 faculty members, including notable members of the National Academy of Medicine. As the largest public medical school in the DC/MD/VA region, faculty-physicians are working to help patients manage chronic diseases like obesity, cancer, heart disease and addiction, while also working on cutting-edge research to address the most critical generational health challenges. In 2024, the School ranked #12 among public medical schools and #27 among all medical schools for R&D expenditures by the National Science Foundation. With a $1.3 billion total operating budget, the School partners with the University of Maryland Medical Center to serve nearly 2 million patients annually. The School's global reach extends around the world with research and treatment facilities in 33 countries. In Maryland, the School of Medicine is spearheading new initiatives in AI and health computing and partnering with the University of Maryland BioPark to develop new medical technologies and bioengineering ventures. For more information, visit medschool.umaryland.edu.
Contact
Jon Kelvey
JKelvey@som.umaryland.edu
