December 02, 2025 | Jon Kelvey
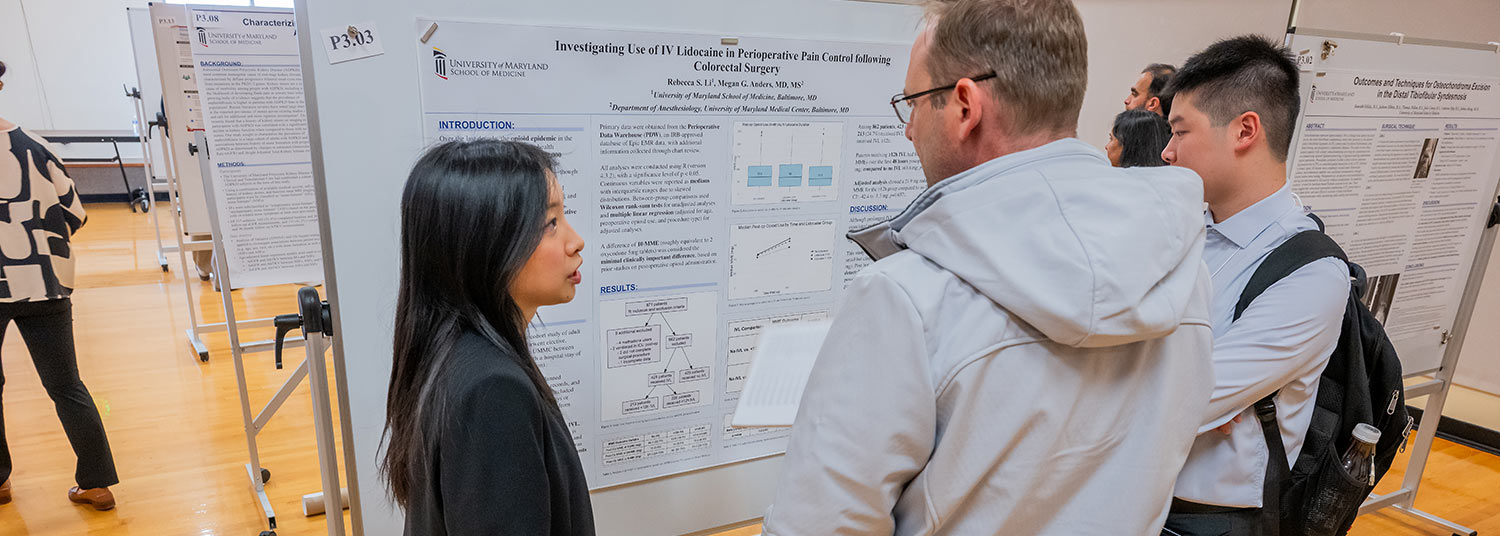
On Nov. 18 and 19, more than 100 University of Maryland School of Medicine (UMSOM) medical students and faculty congregated in the SMC Campus Center for the 48th annual Medical Student Research Day. This year’s group presented on their summer research projects, ranging from comparing treatments for deep vein thrombosis to studying the evolution of pain symptoms over time in patients experiencing subarachnoid hemorrhages.
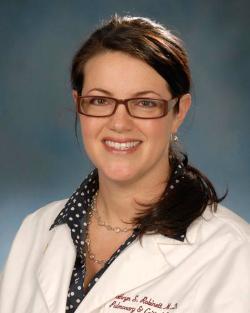 “Medical Student Research Day is an excellent opportunity for our students to network with faculty and build their CVs,” said Kathryn Robinett, MD, UMSOM Associate Professor of Medicine and Associate Dean for Student Research and Education, in her opening remarks. “Another huge benefit is the opportunity to hone their skills in presenting research. Doing research is important, but effectively communicating it is how you obtain grants, publish papers, and inspire others to collaborate.”
“Medical Student Research Day is an excellent opportunity for our students to network with faculty and build their CVs,” said Kathryn Robinett, MD, UMSOM Associate Professor of Medicine and Associate Dean for Student Research and Education, in her opening remarks. “Another huge benefit is the opportunity to hone their skills in presenting research. Doing research is important, but effectively communicating it is how you obtain grants, publish papers, and inspire others to collaborate.”
The annual event continues to expand with 124 students making 142 research presentations, as posters and oral abstracts, compared to just 30 or 40 student participants a little more than a decade ago, according to event organizer Gregory B. Carey, PhD, Associate Professor of Microbiology and Immunology and Assistant Dean for Student Research & Education at UMSOM. “I think this speaks to the dedication of our faculty mentors who invest so much in our students, and the passion and excitement of our students to conduct their own research and engage with others about their work.”
 For her research on deep vein thrombosis, second-year medical student Shaiza Mansoor, ‘28, found a mentor in Brajesh Lal, MBBS, a UMSOM Professor of Surgery and director of both the NIH Vascular Imaging Core Facility and the Center for Vascular Research at the University of Maryland.
For her research on deep vein thrombosis, second-year medical student Shaiza Mansoor, ‘28, found a mentor in Brajesh Lal, MBBS, a UMSOM Professor of Surgery and director of both the NIH Vascular Imaging Core Facility and the Center for Vascular Research at the University of Maryland.
Mansoor's research project looked at whether adding an exercise regimen designed to increase venous blood flow in the legs to the standard anticoagulant treatment for deep vein thrombosis could increase clearance of residual blood clots. She looked at nearly 100 patients who experienced deep vein thrombosis within the past 30 days, randomly assigning half to receive the standard anticoagulants while the other half received these drug plus an exercise regimen involving moderate to vigorous walking on a treadmill for 30 minutes, three times a week, for three months. ”We saw that in the exercise group, 84 percent of patients had over 80 percent of resolution of their residual clot, compared to the control group, which had 73 percent of patients with over 80 percent resolution,” Mansoor said. She is now conducting further analysis of the results, which could potentially support including exercise rehabilitation into the standard of care for treatment following deep vein thrombosis.
 Second-year medical student Ruchika Gadagkar, ‘28, worked with Associate Professor of Neurology Nicholas Morris, MD, for her research on how pain changes over time in patients who have experienced a subarachnoid hemorrhage, where a person bleeds into one of the protective layers of tissue between the skull and brain. “It is characterized as the worst headache of their life by patients,” Gadagkar said.
Second-year medical student Ruchika Gadagkar, ‘28, worked with Associate Professor of Neurology Nicholas Morris, MD, for her research on how pain changes over time in patients who have experienced a subarachnoid hemorrhage, where a person bleeds into one of the protective layers of tissue between the skull and brain. “It is characterized as the worst headache of their life by patients,” Gadagkar said.
Gadagkar surveyed patients at four, 10, 16, 90, and 120 days after their hemorrhage, and found that their headache severity decreased over time. But she also found that at the 90-day follow-up, patients reported an increased prevalence of pain in the extremities, such as the hands and legs. Gadagkar concluded that “a one-size fits all approach for analgesic protocols after a subarachnoid hemorrhage may be misguided,” she said, “especially if the focus is entirely on headache pain without assessing for pain in the extremities."
Gadagkar hopes to conduct research alongside a career focused on the clinic, but isn’t yet sure if neurology is the specialty she will pursue. “I'm also exploring a lot of different specialties, trying to get my feet wet in research wherever I can,” she said.
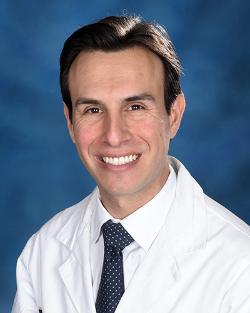
Gadagkar’s strategy fits well with that of the keynote speaker for this year’s Medical Student Research Day, Adam Kaufman, MD, PhD, an Assistant Professor of Otorhinolaryngology-Head & Neck Surgery, who initially wanted to be a neurosurgeon but found success in exploring unconventional opportunities.
”I’ve come to believe that detours are actually the best part,” Dr. Kaufman said in his address. “Where disciplines overlap, where ideas collide, or people think differently from one another; that's where discovery happens.”

Contact
Jon Kelvey
JKelvey@som.umaryland.edu
