August 30, 2022 | Vanessa McMains
University of Maryland School of Medicine researchers demonstrated that a stress response in the brain is essential for ketamine’s antidepressant response in mice suggesting new ways to improve antidepressant therapy for patients who do not respond to the treatment
Many researchers who work with mice can tell you that mice behave differently depending on who is handling them. Anecdotal reports and some existing scientific reports indicate that mice tend to be more fearful and uptight around men, and relaxed and comfortable around women. Whether this behavior actually affects research results though, remains a sort of the elephant in the room that not many people seem to want to address.
Now, researchers at the University of Maryland School of Medicine have shown that mice respond more to the antidepressant effects of the drug ketamine when administered by men and not by women. The group demonstrated that the response of mice detected in a specific region of their brain from handling by a man is essential for ketamine’s effect to work. Then, the researchers identified the mechanism behind this response.

The findings were published on August 30 in Nature Neuroscience.
“Our findings in mice suggests that activating a specific stress circuit in the brain may be a way to improve ketamine treatment. Our thought is that you may be able to provide a more robust antidepressant effect if you combine the ketamine with activation of this brain region, either a drug that spurs this process in the brain or even some sort of specific stressor,” said Todd Gould, MD, Professor of Psychiatry at the University of Maryland School of Medicine.
Dr. Gould’s team anecdotally noticed that ketamine’s antidepressant-like effects only seemed to work consistently when male researchers administered the treatment to mice. The team reached out to other labs studying mouse responses to ketamine, who reported the same issues, but no one had yet systematically documented the phenomena and investigated the cause. At the time, most of Dr. Gould’s team was women and so figuring out why the experiments did not work when women performed them was essential to the team getting workable data, so they could move forward with project.
To look into this, they began by observing mouse preference for being around T-shirts or cotton swabs rubbed on the wrists, elbow, or behind the ear that came from men versus women. The mice preferred spending more time around T-shirts and cotton swabs that came from women rather than men. When the researchers used a chemical to block the smell of the mice, they no longer preferred women’s T-shirts or cotton swabs over men’s.
 “While the influence of the sex of the scientist administering ketamine is not directly relevant to the human response to ketamine, the brain mechanism underlying the findings of this study could help determine why some people do not respond to ketamine antidepressant therapy and suggest ways to potentially make this therapy work better for those patients who do not respond well,” said Mark T. Gladwin, MD, Vice President for Medical Affairs at University of Maryland, Baltimore and the John Z. and Akiko K. Bowers Distinguished Professor and Dean at UMSOM.
“While the influence of the sex of the scientist administering ketamine is not directly relevant to the human response to ketamine, the brain mechanism underlying the findings of this study could help determine why some people do not respond to ketamine antidepressant therapy and suggest ways to potentially make this therapy work better for those patients who do not respond well,” said Mark T. Gladwin, MD, Vice President for Medical Affairs at University of Maryland, Baltimore and the John Z. and Akiko K. Bowers Distinguished Professor and Dean at UMSOM.
Next, they confirmed the original anecdotal findings with a systematic experiment using many researchers to verify that mice responded to ketamine when administered men, but not by women. Then, the researchers wanted to understand the mechanism behind why the mice behave this way. The researchers investigated several factors potentially involved in mediating ketamine’s response in mice, but ultimately settled on one: corticotropin-releasing factor (CRF). CRF is located region of the brain, known as the hippocampus, responsible for learning and memory that had previously been associated with depression. When the researchers had women administer the ketamine along with an injection of CRF, the mice finally responded to ketamine as if they were being treated with an antidepressant.
“We think that some people may have higher or lower levels of CRF, and we believe that people do not respond well to ketamine antidepressant therapy might respond if we could administer the treatment with some CRF-related chemical that could induce ketamine’s effects,” said Polymnia Georgiou, PhD, a former postdoctoral fellow in Dr. Gould’s laboratory, who led the project. “Alternatively, we typically see the antidepressant effects of ketamine lasting 1-3 days, but with CRF administration, it is possible that we may be able to extend the effects to last longer with CRF.”
This work was supported by National Institutes of Health’s National Institute on Mental Health (NIMH) (grants MH107615, MH086828, MH093897), the Veterans Administration (1I01BX004062), and the NIMH and National Institute of Aging Intramural Research Programs.
Author Carlos Zarate, MD, of the NIMH, is a co-inventor on a patent for the use of ketamine in major depression and suicidal ideation. Authors Panos Zanos, PhD, former Assistant Professor of Psychiatry at UMSOM; Jaclyn Highland, PhD, former graduate student at University of Maryland; Ruin Moaddel, PhD, of the National Institute of Aging, Dr. Zarate, and Dr. Gould are co-inventors in patents and patent applications related to the pharmacology and use of (2R,6R)-HNK in the treatment of depression, anxiety, anhedonia, suicidal ideation, and post-traumatic stress disorders. Dr. Moaddel and Dr. Zarate have assigned their patent rights to the U.S. government but will share a percentage of any royalties that may be received by the government. Dr. Zanos, Dr. Highland, and Dr. Gould have assigned their patent rights to the University of Maryland, Baltimore, but will share a percentage of any royalties that may be received by the University of Maryland, Baltimore. Dr. Gould has received research funding from Allergan and Roche Pharmaceuticals and has served as a consultant for FSV7 LLC, during the preceding three years.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world — with 46 academic departments, centers, institutes, and programs, and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.3 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic, and clinically based care for nearly 2 million patients each year. The School of Medicine has nearly $600 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 students, trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of over $6 billion and an economic impact of nearly $20 billion on the state and local community. The School of Medicine, which ranks as the 8th highest among public medical schools in research productivity (according to the Association of American Medical Colleges profile) is an innovator in translational medicine, with 606 active patents and 52 start-up companies. In the latest U.S. News & World Report ranking of the Best Medical Schools, published in 2021, the UM School of Medicine is ranked #9 among the 92 public medical schools in the U.S., and in the top 15 percent (#27) of all 192 public and private U.S. medical schools. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
Contact
Vanessa McMains
Director, Media & Public Affairs
University of Maryland School of Medicine
Institute of Human Virology
vmcmains@ihv.umaryland.edu
Cell: 443-875-6099
Related stories

Tuesday, December 19, 2023
UM School of Medicine Review Highlights Rise in Psychiatric Disorders Linked to Increased Cannabis Use
The widespread use of cannabis (marijuana) and its increased potency are associated with a rise in cannabis-related psychiatric conditions, according to a new University of Maryland School of Medicine (UMSOM) review article that was recently published in the New England Journal of Medicine. It highlights the urgent need for doctors to screen for and treat patients who are experiencing symptoms of cannabis use disorder, which means they are experiencing significant problems from their use of the drug.
Friday, December 08, 2023
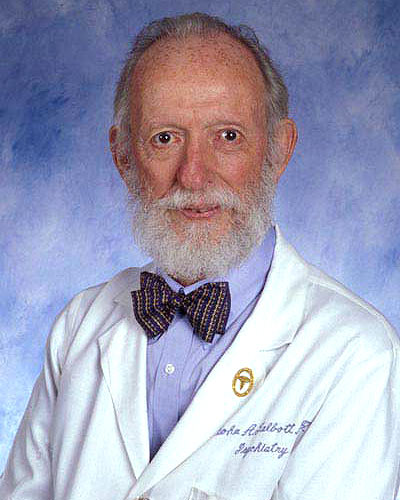
UM School of Medicine Celebrates the Life and Legacy of Former Psychiatry Chair, John A. Talbott, MD
It is with deep sorrow that we announce the news of the passing of internationally renowned psychiatrist John A. Talbott, MD, former Chair of Psychiatry and Professor Emeritus at the University of Maryland School of Medicine (UMSOM).

Friday, January 06, 2023
UM School of Medicine Scientists Create First Extensive Brain Cell Data Repository
Neuroscience researchers now have access to 50 million brain cells to better understand how the brain develops and functions or changes with disease or trauma. Last month, scientists at the University of Maryland School of Medicine’s (UMSOM) Institute for Genome Sciences (IGS) unveiled a “one-stop shop” for brain cell data called the Neuroscience Multi-Omic Archive (NeMO Archive). This archive is now available to neuroscience researchers to transform their understanding of the complex workings of the brain.

Thursday, September 23, 2021
Dr. Deanna Kelly Appointed New Chair of Institutional Review Board for the Maryland Department of Health
Deanna Kelly, PharmD, Professor of Psychiatry at the University of Maryland School of Medicine (UMSOM), has been appointed to lead the prestigious committee of experts who review and approve all proposed research projects involving human participants for the Maryland Department of Health (MDH). She will chair the MDH Institutional Review Board (IRB) for the next four years, a position she started in July.

Wednesday, March 27, 2019
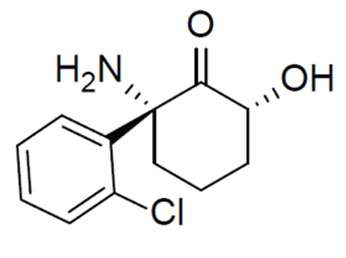
UMSOM Researchers Discover a Critical Receptor Involved in the Response to Fast-Acting Antidepressants Like Ketamine
Effective treatment of clinical depression remains a major mental health issue, with roughly 30 percent of patients who do not respond to any of the available treatments. Researchers at the University of Maryland School of Medicine (UMSOM) have discovered a crucial receptor called mGlu2 that is critical to the mechanism of fast-acting antidepressants such as ketamine when used to treat depression.
Wednesday, June 07, 2017
Dr. Jill RachBeisel Named Vice Chair for Clinical Affairs in UM School of Medicine’s Department of Psychiatry
Bankole A. Johnson, DSc, MD, MBChB, The Dr. Irving J. Taylor Professor and Chair for the Department of Psychiatry, Professor of Pharmacology, Anatomy and Neurobiology, along with UM SOM Dean E. Albert Reece, MD, PhD, MBA, announced today that Jill RachBeisel, MD, Associate Professor of Psychiatry, has been named Vice Chair for Clinical Affairs for the UM SOM Department of Psychiatry, commencing at the start of the next academic year.
Wednesday, May 04, 2016
UM SOM Researchers Identify Potentially Revolutionary Antidepressant Compound
For years, scientists and doctors have known that ketamine can treat depression very rapidly, often working within hours, compared to weeks or months for widely used antidepressants. However, the drug, which is approved as an anesthetic, has major side effects – it is linked to hallucinations and dissociation - a sense of being outside your own body – and for these reasons is abused as a club drug. Not surprisingly, this limits its use in the treatment of depression.