A $7.8 Million Federal Grant Will Fund the Outreach Program, Which Leverages Partnerships with Key Community Leaders Across Four States
 In an effort to increase COVID-19 vaccination rates among children and families, and ultimately help bring the pandemic under control, the Department of Family & Community Medicine (DFCM) and the Department of Psychiatry at the University of Maryland School of Medicine (UMSOM) are partnering with key community and faith-based groups in Baltimore city to reach the most vulnerable and underserved communities. This partnership will also extend across Maryland, Delaware, Virginia, and West Virginia.
In an effort to increase COVID-19 vaccination rates among children and families, and ultimately help bring the pandemic under control, the Department of Family & Community Medicine (DFCM) and the Department of Psychiatry at the University of Maryland School of Medicine (UMSOM) are partnering with key community and faith-based groups in Baltimore city to reach the most vulnerable and underserved communities. This partnership will also extend across Maryland, Delaware, Virginia, and West Virginia.
The Community-based Workforce for COVID-19 Vaccine Outreach Program at UMSOM will support families with children aged 12-15 years old, including those with special behavioral health needs, by addressing barriers to vaccines. It will also provide culturally relevant information, practical support, and one-on-one conversations with trusted community partners about vaccine concerns. The multi-state program is funded by a $7.8 million award from the U.S. Health Resources and Services Administration (HRSA). It builds upon community work already underway by UMSOM that is funded by the Maryland Community Health Resources Commission (MCHRC), which aims to reach individuals in vulnerable communities at the grass roots level across the state.
“It is critical to understand that the objections and concerns about getting vaccinated are real and valid in these communities in order to address them,” said Niharika Khanna, MBBS, MD, DGO, Professor, Department of Family & Community Medicine, Section Chief of Population Health in the Department, and co-principal investigator (PI) for the program. “We must acknowledge them and tailor our conversations accordingly.”
Language and cultural barriers are being addressed by cultural ambassadors and community leadership engagement. Multiple methods of communication are planned, including face to face, virtual, print, live, radio, television, social media, billboards, and other methods. UMSOM’s partners are going into communities that are difficult to reach using a public health messaging truck. Others are reaching the homeless population with street-based outreach and are engaging post-penitentiary populations through behavioral health providers.
 “The regions of the four states that have high rates of vaccine hesitancy are in a variety of settings, including rural and urban communities,” said co-PI Gloria M. Reeves, MD, Associate Professor, Department of Psychiatry at UMSOM, which is partnering with UMSOM's Department of Family and Community Medicine. “Our outreach plans were developed to address specific geographic challenges such as poor internet access, utilize community strengths like coordination with local schools and faith-based organizations, and provide testimonials from community representatives on how they approached vaccine decision making.”
“The regions of the four states that have high rates of vaccine hesitancy are in a variety of settings, including rural and urban communities,” said co-PI Gloria M. Reeves, MD, Associate Professor, Department of Psychiatry at UMSOM, which is partnering with UMSOM's Department of Family and Community Medicine. “Our outreach plans were developed to address specific geographic challenges such as poor internet access, utilize community strengths like coordination with local schools and faith-based organizations, and provide testimonials from community representatives on how they approached vaccine decision making.”
Partnering with Key UMB Programs and Community Leaders
The program incorporates key community partners already trusted in these communities, such as several Area Health Education Centers (AHEC), including the University of Maryland, Baltimore Community Engagement Center (CEC). Other community partners central to this program include the AME Zion Church, the National Association for the Advancement of Colored People (NAACP) Baltimore Branch, Community Behavioral Health, National Federation of Families, and Family Voices. UMSOM’s partnerships with these community leaders will help to identify those with vaccine hesitancy in a wider swath of the population across four states. These partnerships will be used to develop a family, community, and faith-based approach toward ‘enhanced outreach’ in these communities. This is not a one-size-fits-all program.
Based on information collected from community leaders and members of each population, the program will be tailored to meet the specific religious, ethnic, and socioeconomic needs of each community.
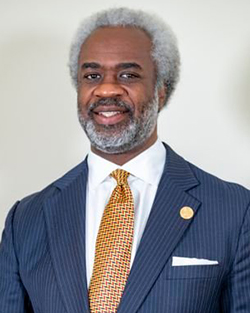 “Through this HRSA-funded collaboration with UMB and other partners, we will be able to help our communities to overcome vaccine hesitancy by initiating conversations about the very real and certain consequences of COVID, including hospitalization, long-term disability, and death," said Rev. Kobi Little of the Baltimore NAACP.
“Through this HRSA-funded collaboration with UMB and other partners, we will be able to help our communities to overcome vaccine hesitancy by initiating conversations about the very real and certain consequences of COVID, including hospitalization, long-term disability, and death," said Rev. Kobi Little of the Baltimore NAACP.
"The vaccines are our best shot at staying safe,” Little said. “By engaging in frank and honest conversations with friends, family, and neighbors at the grass roots level, we hope to activate communities to lead efforts to protect our people and get everyone vaccinated."
The goal in Baltimore is to address social barriers to COVID-19 vaccines and develop strategies and infrastructure to address vaccine hesitancy in Baltimore city zip codes that have neighborhoods where roughly 70 percent of the population has not been vaccinated. The program will also tap into synergies with the NAACP, AME Zion Church, and the Central AHEC to address the need in Baltimore for community outreach and engagement. The DFCM is partnering with the SEED school in Baltimore to provide vaccination, education, and outreach to parents, students, and school staff. The central AHEC will provide navigation and “post-vaccine care packages.”
Community Outreach Through Largest HRSA Award in Maryland to reach Vulnerable Communities
A key component to the program involves hiring and mobilizing community outreach workers and family peer specialists (FPS), who will serve as trusted messengers to support families in one-to-one relationships. It will also include community health workers, social support specialists, and others to increase vaccine access for the hardest-hit and highest-risk communities through high-touch, on-the-ground outreach to educate and assist individuals in getting the information they need about vaccinations.
UMSOM is one of 14 recipients of funding from HRSA for the $125 million community-based program announced in June by the Biden-Harris Administration. It is the largest of two awards granted in Maryland.
A Data-Based Approach Toward Reaching Vulnerable Communities
Dr. Khanna has been tracking patient data in vulnerable communities, with the intent of gaining a greater understanding of COVID-19 and how it has impacted patient care. This data tracking helped set the stage to better direct future healthcare directives, re-purpose clinical teams, redesign workflows, ensure optimal patient care for those with COVID-19, and to bring them into or continue primary care. In particular, her team focused on Family Medicine patients largely from West Baltimore as a baseline for building a deeper insight about patient symptoms and transmission.
Armed with this information, Dr. Khanna and her team began publishing a monthly COVID-19 Dashboard, which includes a number of data-based perspectives on the emerging trends in unique COVID-19 cases by race, age, and sex. Since the start of vaccination for COVID-19, they also tracked vaccination trends in patients with data collected in the Chesapeake Regional Information System (CRISP), the designated Health Information Exchange in Maryland and the District of Columbia. In addition, the team focused on age, race, chronic disease, and socioeconomic predictors of health.
 A particular area of interest was socioeconomic factors and how they intersect with COVID-19, for which Dr. Khanna and her team used the Area Deprivation Index (ADI) intensity map. The ADI incorporates census data to rank neighborhoods by socioeconomic disadvantage in a region of interest. The resulting data revealed that the most pandemic-vulnerable Family Medicine patients were African Americans living in highly deprived areas within densely populated multi-housing units, followed by whites living in areas with low or intermediate ADI ranks.
A particular area of interest was socioeconomic factors and how they intersect with COVID-19, for which Dr. Khanna and her team used the Area Deprivation Index (ADI) intensity map. The ADI incorporates census data to rank neighborhoods by socioeconomic disadvantage in a region of interest. The resulting data revealed that the most pandemic-vulnerable Family Medicine patients were African Americans living in highly deprived areas within densely populated multi-housing units, followed by whites living in areas with low or intermediate ADI ranks.
“This community-based approach is built on our close connections within these communities and is supported by data generated by our own faculty, setting the path toward fighting the COVID-19 pandemic in the broadest way possible.,” said E. Albert Reece, MD, PhD, MBA, Executive Vice President for Medical Affairs, UM Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor and Dean, University of Maryland School of Medicine. “We know that vaccines are our best defense against this deadly virus, and they are even more important as we are seeing a rise in cases with new variants.”
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 46 academic departments, centers, institutes, and programs, and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.2 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically based care for nearly 2 million patients each year. The School of Medicine has nearly $600 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 students, trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of over $6 billion and an economic impact of nearly $20 billion on the state and local community. The School of Medicine, which ranks as the 8th highest among public medical schools in research productivity (according to the Association of American Medical Colleges profile) is an innovator in translational medicine, with 606 active patents and 52 start-up companies. In the latest U.S. News & World Report ranking of the Best Medical Schools, published in 2021, the UM School of Medicine is ranked #9 among the 92 public medical schools in the U.S., and in the top 15 percent (#27) of all 192 public and private U.S. medical schools. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu

