February 22, 2023 | Vanessa McMains
Findings Will Direct Researchers to Risk Genes in Predisposed Patients
When the artery that supplies the stomach and the liver forms a bulge that ruptures, this medical emergency results in the deaths of 50 percent of patients before they reach the hospital. This “silent killer” condition, known as abdominal aortic aneurysm, led to the death of Albert Einstein — and is responsible for nearly 5,000 deaths in the U.S. each year. Now researchers have found new clues that eventually could lead to earlier detection methods to save lives in the future.
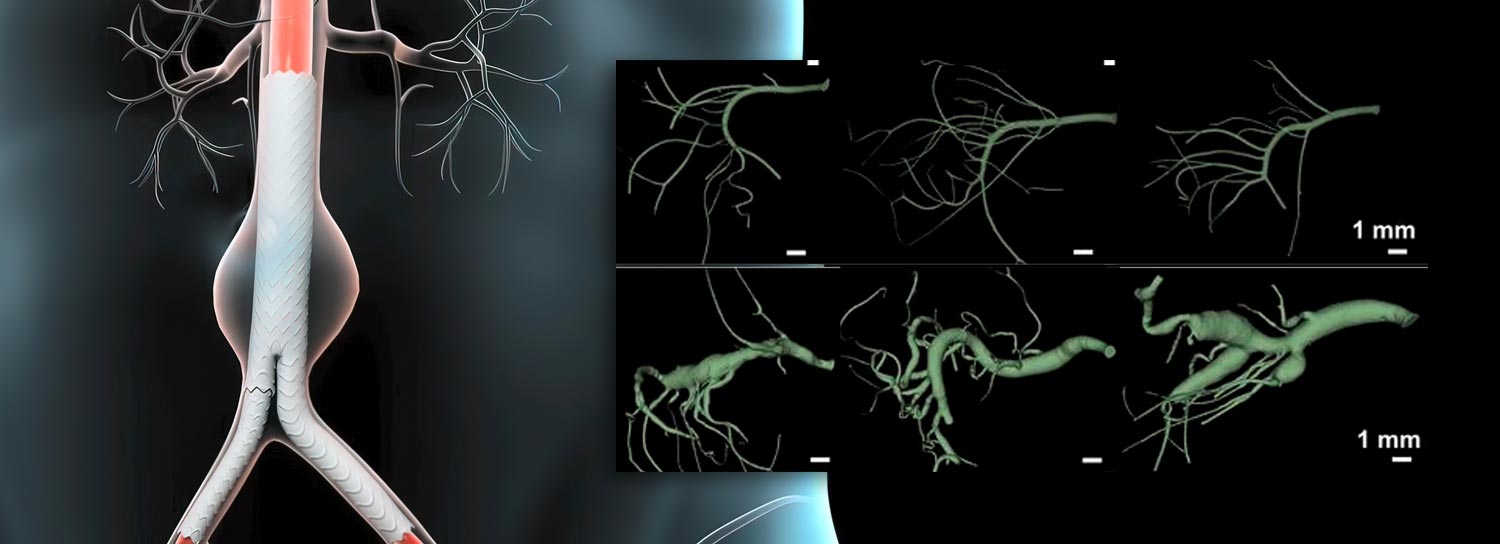
 Surgery can prevent abdominal aneurysms by inserting a tube inside the damaged artery, but physicians do not have a way to predict who is most at risk and should be screened for this condition. Unlike the more common thoracic aortic aneurysms which occur in the chest, abdominal aneurysms do not have any known genetic risk factors.
Surgery can prevent abdominal aneurysms by inserting a tube inside the damaged artery, but physicians do not have a way to predict who is most at risk and should be screened for this condition. Unlike the more common thoracic aortic aneurysms which occur in the chest, abdominal aneurysms do not have any known genetic risk factors.
In a new study using mice, University of Maryland School of Medicine (UMSOM) researchers were able to tease apart the molecular components involved in abdominal aneurysms to better understand how and why they form.
The findings were published on January 24, 2023, in JCI Insight.
“Our next step is to conduct human genetic studies on these newly identified mice components to see if we can find a genetic correlation in abdominal aneurysm patients. My gut feeling says that we will identify previously unknown genetic mutations associated with an increased risk of this condition,” said study leader Dudley Strickland, PhD, Professor of Surgery and Physiology, Director of the Center for Vascular & Inflammatory Diseases at UMSOM. “From there, we could screen people to identify those with an increased risk of developing abdominal aneurysms, have their physicians monitor them, and intervene when necessary to save lives.”
Having high cholesterol or high blood pressure, and being older, a smoker, or a man can increase one’s odds of developing an abdominal aneurysm. Abdominal aneurysms usually are caused by plaque buildup in the arteries, but infection or injury can also cause this condition, according to the Centers for Disease Control and Prevention.
“Certain genetic mutations may make someone more likely to have their repair process end up going haywire causing the portion of the artery to swell like a balloon and instead of healing a section of damaged artery,” said study co-author Jackie Zhang, MD, Surgery Resident at UMSOM and researcher in Dr. Strickland’s laboratory, who was funded from a training grant from the National Heart, Lung, and Blood Institute (NHLBI) for this study.
To conduct the study, the research team decided to focus on the protein LRP1, since it is involved in thoracic aortic aneurysms. To test this, they genetically engineered mice that did not have LRP1 in the cells that line blood vessels known as smooth muscle cells. Using CT scans to look at these blood vessels without LRP1, the researchers noticed that the abdominal arteries were abnormally enlarged as compared to vessels in normal mice.
 Next, using a highly sophisticated comparative protein analysis of normal and diseased tissue, they found that the enlarged blood vessels in the genetically engineered mice had higher levels of proteins involved in the hormonal angiotensin-renin system that regulates blood pressure and blood vessel growth and development. For the final part of the study, the researchers were able to prevent the abdominal arteries from enlarging in the engineered mice when they blocked an angiotensin receptor using the blood pressure drug losartan. They also prevented the enlarged arteries by removing a precursor of the angiotensin hormone in the liver of mice, further demonstrating the connection between LRP1 and the angiotensin-renin system in aneurysm development.
Next, using a highly sophisticated comparative protein analysis of normal and diseased tissue, they found that the enlarged blood vessels in the genetically engineered mice had higher levels of proteins involved in the hormonal angiotensin-renin system that regulates blood pressure and blood vessel growth and development. For the final part of the study, the researchers were able to prevent the abdominal arteries from enlarging in the engineered mice when they blocked an angiotensin receptor using the blood pressure drug losartan. They also prevented the enlarged arteries by removing a precursor of the angiotensin hormone in the liver of mice, further demonstrating the connection between LRP1 and the angiotensin-renin system in aneurysm development.
“Now that the researchers identified some of the components involved in these aneurysms, they will next need to explore how they interact together,” said UMSOM Dean Mark T. Gladwin, MD, Vice President for Medical Affairs, University of Maryland, Baltimore, and the John Z. and Akiko K. Bowers Distinguished Professor. “For example, it’s known that LRP1 is involved in transporting proteins from outside the cell to the inside in the region of the cell that digests and recycles those materials, but we do not know how that plays a role in forming or preventing aneurysms.”
This study was supported by grants from the NHLBI (R35HL135743, R35HL155649, F32HL131293, 1K08HL146893-01, and T32HL007698), the American Heart Association (AHA 15SGF24470170), and the Strategically Focused Research Network in Vascular Disease.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world — with 46 academic departments, centers, institutes, and programs, and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.3 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic and clinically based care for nearly 2 million patients each year. The School of Medicine has nearly $600 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 students, trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of over $6 billion and an economic impact of nearly $20 billion on the state and local community. The School of Medicine, which ranks as the 8th highest among public medical schools in research productivity (according to the Association of American Medical Colleges profile) is an innovator in translational medicine, with 606 active patents and 52 start-up companies. In the latest U.S. News & World Report ranking of the Best Medical Schools, published in 2021, the UM School of Medicine is ranked #9 among the 92 public medical schools in the U.S., and in the top 15 percent (#27) of all 192 public and private U.S. medical schools. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit www.medschool.umaryland.edu
Contact
Vanessa McMains
Director, Media & Public Affairs
University of Maryland School of Medicine
Institute of Human Virology
vmcmains@ihv.umaryland.edu
Cell: 443-875-6099
Related stories
Friday, July 29, 2022
New Study Provides Insight for How Congenital Heart Defects Manifest
About one percent of the world population is born with a congenital heart defect, which affects about 40,000 U.S. births each year, but how these particular birth defects come about is largely unknown.

Tuesday, October 04, 2016
UM SOM Launches Unprecedented Initiatives to Create New Generation of Research Scientists Among Students, Trainees and Faculty
New and expanded research development programs at the University of Maryland School of Medicine will include focus on developing junior, minority and female faculty investigators as well as students and trainees.