August 24, 2022 | Heide Aungst
Findings Could Lead to Treatments for a Variety of Conditions
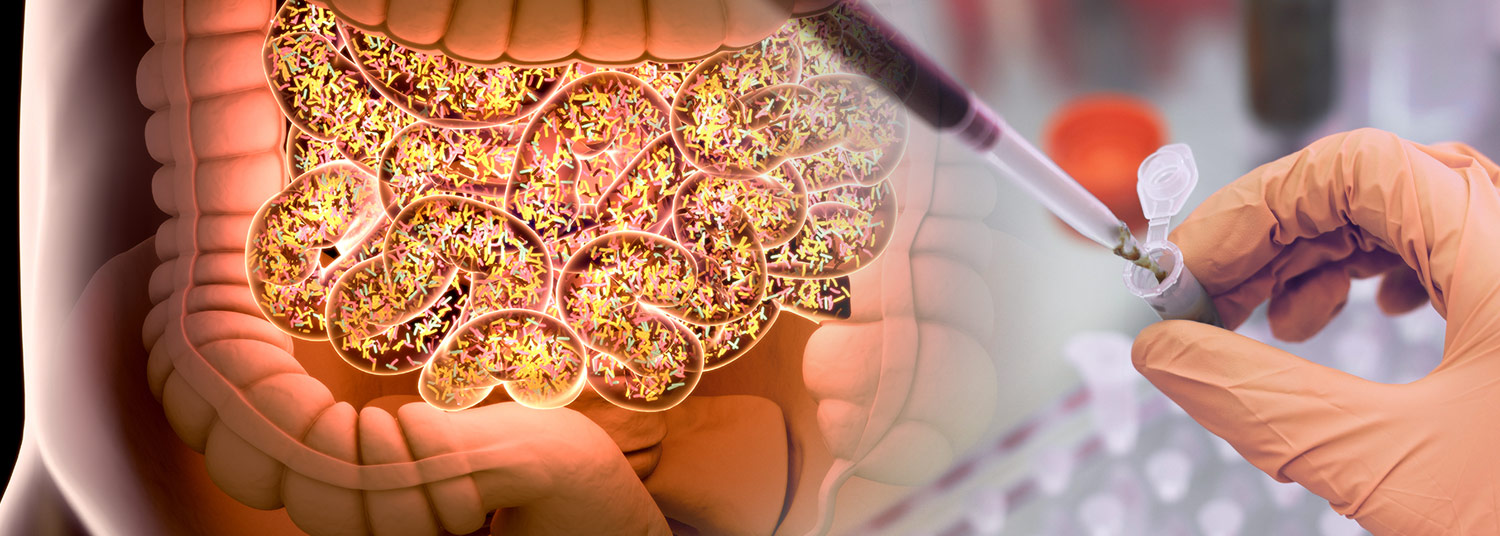
Fecal transplants have been successful in treating serious diarrheal infections but have often failed when tried with other diseases. Up until now, no one could predict why these treatments sometimes failed to help restore healthy bacteria in the colon. Researchers from the University of Maryland School of Medicine’s (UMSOM) Institute for Genome Sciences (IGS) have discovered important clues that could lead more personalized approaches to optimize treatment success. They published their findings in Cell Reports Medicine online earlier this month.
Fecal microbial transplantation is a procedure in which fecal matter, or stool, is collected from a healthy donor and placed into the gastrointestinal tract of a patient. It has been well studied as a cure for serious diarrheal infections, such as C. difficile infection, as well as many other conditions, including obesity. In fecal transplants, doctors hope that the good microbes from the donor will multiply and rid the gut of bacteria causing the disease in the patient.
 Despite numerous studies, little has been known about the mechanisms that make them work—or fail, in some cases. The latest finding may prove to be a model that could be used to make fecal transplants more successful, so that researchers and clinicians can discover if they help a particular condition, like obesity, or gastrointestinal disease, such as irritable bowel syndrome.
Despite numerous studies, little has been known about the mechanisms that make them work—or fail, in some cases. The latest finding may prove to be a model that could be used to make fecal transplants more successful, so that researchers and clinicians can discover if they help a particular condition, like obesity, or gastrointestinal disease, such as irritable bowel syndrome.
“It’s important to view the gut microbiome as an ecosystem,” said lead author W. Florian Fricke, PhD, Adjunct Assistant Professor of Microbiology and Immunology at UMSOM and a scientist at IGS. He is also a Professor at the University of Hohenheim in Stuttgart, Germany. “We set out to better understand the microbiome’s assembly process within that ecosystem. In other words, we would like to identify what mechanism allows the donor’s microbiota strains to grow and overtake the patient’s strains to create a balanced and healthy gut.”
The goal of a fecal transplant is “engraftment” of the donor’s microbiota into the patient, which means the donor microbiota strains replace the patient’s own microbiota strains. This generally has worked well as a cure for a C. difficile infection, where one strain of bacteria causes severe diarrhea, but it has had far less success for other gastrointestinal conditions. Clinical trials using fecal transplants to treat inflammatory bowel disease, ulcerative colitis, cancer, or obesity have brought disappointing results.
To discover why, Dr. Fricke and his colleagues examined data from 14 fecal transplant trials that included more than 250 patients. They used metagenomics—a process that sequences all genes and genomes from a mixed community at once—to determine the origin of the strains in each patient following transplant. They wanted to see whether patients incorporated the donor strains into their microbiome.
“What we discovered is that the success of a fecal transplant depends on the content and imbalance of the recipient’s gut microbes going into the transplant,” Dr. Fricke said. “The more disrupted the patient’s gut is, the better it engrafts the donor’s microbiota. The good news is that we can clinically replicate that imbalance with a combination of antibiotics and washing out the colon prior to transplant.”
The lack of a disruption may be a key reason that fecal transplants have not worked as well in curing other specific diseases as it has in treating C. difficile, said Dr. Fricke. Another is the microbiota transferred from a donor needs to be carefully matched to a patient. Donor strains should be selected for their strength to keep harmful bacteria in check and their ability to compete against and overtake any strains that may remain inside the patient.
This study was supported by funding from the German Research Foundation, the Austrian Science Fund, a Science Foundation Ireland Centre grant, and a Science Foundation Ireland professorship. Researchers from the University of Hohenheim, Medical University of Graz, University of Sydney, and the University College Cork also co-authored this study.
The authors have no conflicts of interest.
About the University of Maryland School of Medicine
Now in its third century, the University of Maryland School of Medicine was chartered in 1807 as the first public medical school in the United States. It continues today as one of the fastest growing, top-tier biomedical research enterprises in the world -- with 46 academic departments, centers, institutes, and programs, and a faculty of more than 3,000 physicians, scientists, and allied health professionals, including members of the National Academy of Medicine and the National Academy of Sciences, and a distinguished two-time winner of the Albert E. Lasker Award in Medical Research. With an operating budget of more than $1.3 billion, the School of Medicine works closely in partnership with the University of Maryland Medical Center and Medical System to provide research-intensive, academic, and clinically based care for nearly 2 million patients each year. The School of Medicine has nearly $600 million in extramural funding, with most of its academic departments highly ranked among all medical schools in the nation in research funding. As one of the seven professional schools that make up the University of Maryland, Baltimore campus, the School of Medicine has a total population of nearly 9,000 faculty and staff, including 2,500 students, trainees, residents, and fellows. The combined School of Medicine and Medical System (“University of Maryland Medicine”) has an annual budget of over $6 billion and an economic impact of nearly $20 billion on the state and local community. The School of Medicine, which ranks as the 8th highest among public medical schools in research productivity (according to the Association of American Medical Colleges profile) is an innovator in translational medicine, with 606 active patents and 52 start-up companies. In the latest U.S. News & World Report ranking of the Best Medical Schools, published in 2021, the UM School of Medicine is ranked #9 among the 92 public medical schools in the U.S., and in the top 15 percent (#27) of all 192 public and private U.S. medical schools. The School of Medicine works locally, nationally, and globally, with research and treatment facilities in 36 countries around the world. Visit medschool.umaryland.edu
About the Institute for Genome Sciences
The Institute for Genome Sciences (IGS) at the University of Maryland School of Medicine has revolutionized genomic discoveries in medicine, agriculture, environmental science, and biodefense since its founding in 2007. IGS investigators research areas of genomics and the microbiome to better understand health and disease, including treatments, cures, and prevention. IGS investigators also lead the development of the new field of microbial forensics. IGS is a leading center for major biological initiatives currently underway including the NIH-funded Human Microbiome Project (HMP) and the NIAID-sponsored Genomic Sequencing Center for Infectious Diseases (GSCID). Follow us on Twitter @GenomeScience.
Contact
Heide Aungst
HAungst@som.umaryland.edu
216-970-5773 (cell)
Related stories
Friday, July 25, 2025
New Research Simulates Cancer Cell Behavior
In the same vein as weather forecast models that predict developing storms, researchers now have developed a method to predict the cell activity in tissues over time. The new software combines genomics technologies with computational modeling to predict cell changes in behavior, such as communication between cells that could cause cancer cells to flourish.

Wednesday, November 06, 2024
Genomic Databases Need More Diversity
It is commonly known that most genomic databases are biased toward people with European ancestry. Scientists have warned that leaving out other populations could skew results in areas such as drug development, diagnostic testing, and polygenic risk scores—which looks at many genetic variations in a person’s DNA to predict their disease risk.

Wednesday, August 28, 2024
Leading Computational Scientist and Oncology Researcher Elana Fertig, PhD, Appointed as New Director of the Institute for Genome Sciences at the University of Maryland School of Medicine
University of Maryland School of Medicine (UMSOM) Dean Mark T. Gladwin, MD, announced today the appointment of Elana J. Fertig, PhD, FAIMBE, as the new Director of the School’s Institute for Genome Sciences (IGS). She is an internationally-recognized researcher known for her work in integrating spatial multi-omics technologies with mathematical models to develop a new predictive medicine paradigm in cancer. Spatial technologies allow researchers to learn about any cell type inside of natural tissue, including gene activity and cell interactions.
Monday, July 18, 2022
New Genomic Research Shows Why Testing Malaria Vaccines in the Clinic is as Rigorous as Natural Exposure in the Field
Malaria is the deadliest mosquito-borne parasitic infection of humans. In 2021, after a century of research, the World Health Organization (WHO) approved the world’s first malaria vaccine. That vaccine reduces the incidence of malaria infections in young children aged 5-17 months by only 30 percent, meaning that it remains critical to continue developing and testing more effective vaccines.

Thursday, March 18, 2021
UM School of Medicine Helps Maryland Conduct State-Wide Sequencing of Variants in Positive COVID-19 Test Specimens
In an effort to monitor the spread of COVID-19 variants in the State of Maryland, University of Maryland School of Medicine (UMSOM) Dean E. Albert Reece, MD, PhD, MBA, announced that UMaryland Genomics at UMSOM will perform genome sequencing of variants in at least 10 percent of COVID-19 test samples, reaching an important benchmark set by the federal government to help control the spread of these variants.

Thursday, February 25, 2021
UM School of Medicine Researchers Participate in Landmark Study Detailing Sequencing of Full Human Genomes to Better Capture Genetic Diversity
Researchers at the University of Maryland School of Medicine (UMSOM) co-authored a study, published today in the journal Science, that details the sequencing of 64 full human genomes. This reference data includes individuals from around the world and better captures the genetic diversity of the human species. Among other applications, the work will enable population-specific studies on genetic predispositions to human diseases as well as the discovery of more complex forms of genetic variation.

Wednesday, February 26, 2020
Researchers Develop First Catalogue of Genes that Comprise Community of Microbes in Vaginal Microbiome
University of Maryland School of Medicine’s (UMSOM) Institute for Genome Sciences (IGS) researchers have created the first catalogue of genes that comprise the community of microbes, which inhabit the human vagina. The catalogue, called human vaginal non-redundant gene catalog (VIRGO), was recently released as a public resource that can be used by researchers to facilitate a more in-depth understanding of the role of vaginal microorganisms in women’s health and to potentially develop future treatments for certain gynecologic conditions.

Tuesday, December 03, 2019
UM School of Medicine Researchers Institute for Genome Sciences' Researchers Discover Potential New Treatment for Tropical Parasitic Disease Using Genomics
Using innovative RNA sequencing techniques, researchers at the University of Maryland School of Medicine (UMSOM) Institute for Genome Sciences identified a promising novel treatment for lymphatic filariasis, a disabling parasitic disease that is difficult to treat. The potential new therapy is an experimental cancer drug called JQ1 and targets proteins found prominently in the worm’s genome; it appears to effectively kill the adult worms in a laboratory setting, according to the study which was published today in the journal mSystems.
Wednesday, May 25, 2016
UMSOM Researchers Develop New Way to Decode Large Amounts of Biological Data
A University of Maryland School of Medicine researcher has helped develop an innovative computing technique that, on very large amounts of data, is both faster and more accurate than current methods. To spur research, a program using this technique is being offered for free to the biomedical research community.