Ventricular Septal Defects (VSDs)
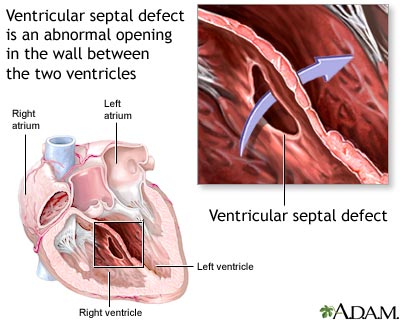 A ventricular septal defect (VSD) is the most common type of congenital heart defect. The wall between the two pumping chambers (ventricles), or ventricular septum, does not form correctly, leaving a hole, or ventricular septal defect (VSD). The hole can be in different locations in the ventricular septum and can be many different sizes.
A ventricular septal defect (VSD) is the most common type of congenital heart defect. The wall between the two pumping chambers (ventricles), or ventricular septum, does not form correctly, leaving a hole, or ventricular septal defect (VSD). The hole can be in different locations in the ventricular septum and can be many different sizes.
VSDs are usually diagnosed with an echocardiogram, or ultrasound of the heart. This can be discov-ered before birth, but is sometimes not noted until after birth. Because VSDs can be associated with genetic syndromes, your perinatalogist may recommend other prenatal testing. VSDs do not have an effect on babies before birth. Most babies do very well right after birth. If the baby does not have any other medical problems, the baby should be able to stay with you after birth. An echocardiogram will be done to confirm the diagnosis. The baby would be discharged with you and come back for follow-up appointments. If there are other issues, or if there are any problems after birth, the baby will go to the neonatal intensive care unit. The baby would be stabilized and an echocardiogram would be done.
Click Here for a PDF Handout
Atrioventricular Septal Defects (AVSDs)
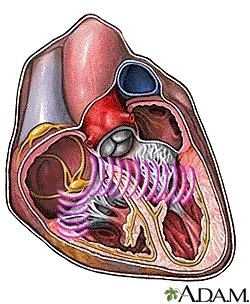
An atrioventricular septal defect (AVSD) is a congenital heart defect. It is also referred to as a atrioventricular (or AV) canal or an endocardial cushion defect. One area of the heart does not develop cor-rectly, and this leads to the several issues. The wall between the two bottom pumping chambers (ventricles), or ventricular septum, does not form correctly, leaving a hole, or ventricular septal defect (VSD). There is also a hole between the two top collecting chambers (atria), called an atrial septal defect (ASD). There are normally two valves which divide the atria from the ventricles, allowing blood to go from the atria into the ventricles, called a tricuspid and a mitral valve. In AVSD’s there is one large valve (common AV valve) that divides the atria and the ventricles.
AVSDs are usually diagnosed with an echocardiogram, or ultrasound of the heart. This can be discovered before birth, but is sometimes not noted until after birth. Because AVSDs can be associated with genetic syndromes, particularly Down syndrome, your perinatalogist may recommend other prenatal testing. AVSDs do not usually have an effect on babies before birth. Most babies do very well right af-ter birth. If the baby does not have any other medical problems, the baby should be able to stay with you after birth. An echocardiogram will be done to confirm the diagnosis. The baby would be dis-charged with you and come back for follow-up appointments. If there are other issues, or if there are any problems after birth, the baby will go to the neonatal intensive care unit. The baby would be stabilized and an echocardiogram would be done. Babies with AVSDs will eventually need to have heart surgery, usually between 3-6 months of age.
Click Here for a PDF Handout
Tetralogy of Fallot (TOF)
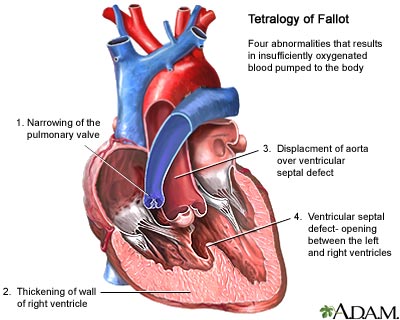 Tetralogy of Fallot (TOF) is a congenital heart defect. TOF is described as 4 abnormalities that occur together. One is that there is a large hole in the wall of muscle (septum) that divides the 2 bottom pump-ing chambers (ventricles) of the heart. That hole is called a ventricular septal defect (VSD). Because of the location of the VSD, two other abnormalities occur. One is that the large blood vessel which takes the blood to the body (aorta) is pulled forward, and “overrides” the ventricular septum so that it sits over both the left and right ventricles; this is called an overriding aorta. The other abnormality that happens is that the abnormally placed muscle causes obstruction to the blood flowing out of the right ventricle and across the pulmonary valve. The right ventricular outflow tract obstruction, can be due to obstruction below the valve, at the valve or in the pulmonary arteries as they deliver blood out to the lungs. The most extreme for on TOF is referred to as pulmonary atresia, because in those patients there is no func-tional pulmonary valve. The right ventricular outflow obstruction leads to thickening of the right ventricle, or right ventricular hypertrophy.
Tetralogy of Fallot (TOF) is a congenital heart defect. TOF is described as 4 abnormalities that occur together. One is that there is a large hole in the wall of muscle (septum) that divides the 2 bottom pump-ing chambers (ventricles) of the heart. That hole is called a ventricular septal defect (VSD). Because of the location of the VSD, two other abnormalities occur. One is that the large blood vessel which takes the blood to the body (aorta) is pulled forward, and “overrides” the ventricular septum so that it sits over both the left and right ventricles; this is called an overriding aorta. The other abnormality that happens is that the abnormally placed muscle causes obstruction to the blood flowing out of the right ventricle and across the pulmonary valve. The right ventricular outflow tract obstruction, can be due to obstruction below the valve, at the valve or in the pulmonary arteries as they deliver blood out to the lungs. The most extreme for on TOF is referred to as pulmonary atresia, because in those patients there is no func-tional pulmonary valve. The right ventricular outflow obstruction leads to thickening of the right ventricle, or right ventricular hypertrophy.
Because TOF can be associated with genetic syndromes, particularly Down syndrome and DiGeorge syndrome, your perinatalogist may recommend other prenatal testing. Before birth, babies are not gen-erally affected by this heart defect. Because babies don’t use their lungs to get oxygen before they are born, they don’t need to send much blood to their lungs. After birth, the symptoms that the baby has will depend on how much obstruction there is to getting blood to the lungs. All babies with TOF need to have surgery to address the defect. Some babies will need surgery soon after birth, but if their oxygen levels are high enough, they may be able to wait until they are 4-6 months old.
Click Here for a PDF Handout
Coarctation of the aorta
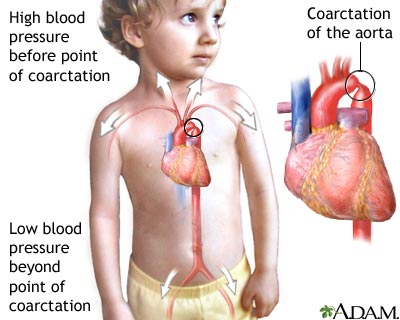 Coarctation of the aorta is a congenital heart defect. It is a narrowing in the aorta, which is the large blood vessel that delivers blood from the heart to the rest of the body. The aorta delivers blood to the upper body, then curves like a candy cane and dives down to the lower body. The narrowing in coarctation occurs in the area after the blood vessels go to the upper body and before the aorta goes down to the lower body.
Coarctation of the aorta is a congenital heart defect. It is a narrowing in the aorta, which is the large blood vessel that delivers blood from the heart to the rest of the body. The aorta delivers blood to the upper body, then curves like a candy cane and dives down to the lower body. The narrowing in coarctation occurs in the area after the blood vessels go to the upper body and before the aorta goes down to the lower body.
Because coarctation can be associated with genetic syndromes, your perinatalogist may recommend other prenatal testing. It can also be seen in patients who have more complex heart disease. The most common abnormality seen with coarctation is a bicuspid aortic valve, or an abnormality of the valve be-tween the left ventricle (pumping chamber) and the aorta. Bicuspid means that there are 2 leaflets of the valve instead of the normal 3 leaflets. Patients with coarctation may have relatives with similar heart defects.
Coarctation can be a difficult diagnosis before birth because of differences in the blood flow patterns. There may be some findings on a fetal echocardiogram which suggest that there may be a coarctation (right side of the heart is larger than the left, aorta is smaller than the pulmonary artery), but sometimes we can only tell for sure with an echocardiogram after the baby is born. If your baby has coarctation of the aorta, surgery is typically done before discharge home from the hospital.
Click Here for a PDF Handout
Transposition of the great arteries (TGA)
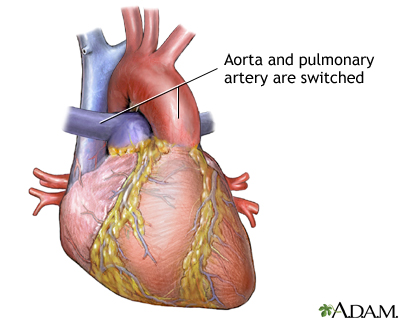 Transposition of the great arteries (TGA) is a congenital heart defect in which the large blood vessels which carry blood from the heart to the lungs (pulmonary arteries) and body (aorta) are coming off the wrong pumping chambers (ventricles). In the normal situation, the pulmonary artery comes from the right ventricle and carries blue blood (less oxygen) to the lungs, and the aorta comes from the left ventricle and carries red blood (more oxygen) to the body. In TGA the aorta comes from the right ventricle and the pulmonary arteries come from the left ventricle.
Transposition of the great arteries (TGA) is a congenital heart defect in which the large blood vessels which carry blood from the heart to the lungs (pulmonary arteries) and body (aorta) are coming off the wrong pumping chambers (ventricles). In the normal situation, the pulmonary artery comes from the right ventricle and carries blue blood (less oxygen) to the lungs, and the aorta comes from the left ventricle and carries red blood (more oxygen) to the body. In TGA the aorta comes from the right ventricle and the pulmonary arteries come from the left ventricle.
Babies with these types of heart defects will need evaluation and stabilization in the neonatal intensive care unit after birth. For this reason, we usually try to plan an induction or C-section for delivery. The diagnosis will be confirmed with an echocardiogram, and babies may get large IV’s placed. Some babies need a breathing tube placed to help manage their condition. The immediate treatment for newborns with TGA is to find a way for the blood to mix, so that the blood getting to the body will have at least some oxygen in it. The baby may need a procedure right after birth and will definitely need surgery before discharge home.
Click Here for a PDF Handout
Single ventricle heart defects
A single ventricle congenital heart defect is the general name for many types of heart defects that result in having one functional ventricle, or pump. In some cases, one of the ventricles is hypoplastic, or small. In other situations, one of the valves that lets blood enter into the ventricles is missing (atresia) or does not let much blood go across it (stenosis). Some of the specific types of single ventricle congenital heart defects include: tricuspid atresia with ventricular septal defect, double inlet left ventricle, unbalanced atrioventricular septal defect, hypoplastic left heart syndrome. There are many other specific diagnoses that are classified as single ventricle congenital heart defects, but the main thing that brings them together is that instead of two ventricles, one to pump to the lungs and one to pump to the body, there is only one usable pump.
Single ventricle heart defects can be associated with genetic problems, so your perinatalogist may recommend other prenatal testing. Babies typically do not have any problems before birth, but may need stabilization soon after birth. For this reason, we usually try to plan an induction or C-section for delivery. Depending on the specific type of single ventricle heart defect, your baby may need surgery before discharge home, as well as other surgeries later in childhood.
Click Here for a PDF Handout
Hypoplastic left heart syndrome (HLHS)
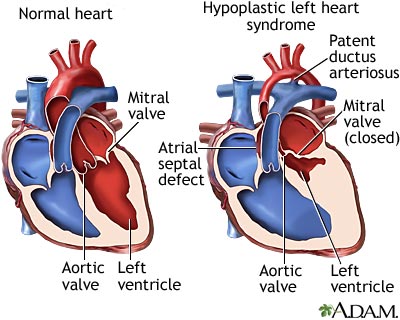 Hypoplastic left heart syndrome (HLHS) is a congenital heart defect in which the left side of the heart is small, or hypoplastic. The left ventricle, mitral valve, aortic valve and aorta are all under developed, and the left side of the heart is unable to send enough blood to the body. This results in the left side of the heart being unable to support the circulation needed by the body's organs.
Hypoplastic left heart syndrome (HLHS) is a congenital heart defect in which the left side of the heart is small, or hypoplastic. The left ventricle, mitral valve, aortic valve and aorta are all under developed, and the left side of the heart is unable to send enough blood to the body. This results in the left side of the heart being unable to support the circulation needed by the body's organs.
HLHS can be associated with genetic problems, so your perinatalogist may recommend other prenatal testing. Babies with these types of heart defects will need evaluation and stabilization in the neonatal intensive care unit after birth. For this reason, we usually try to plan an induction or C-section for delivery. Your baby will need heart surgery before discharge home, as well as other surgeries later in childhood.
Click Here for a PDF Handout
