The UMB Post[doc]
June 2020
Introduction
Dear Readers,
We are very excited to welcome you to our monthly newsletter, The UMB Post[doc].
You will find this newsletter filled with a lot of great information about what’s happening at UMB, science news, career development info, conversations with experts, UMB alumni, nerdy humor, etc.
Whether you are a seasoned scientist or a young investigator, we hope you find something in this newsletter that speaks to you. If you like what you see or have ideas about what else you would like to see here, do reach out to us. If you would like to be added to the mailing list for this newsletter, please fill out the following form.
To the first of many issues to come!
Best,
The UMB Post[Doc] Editorial Team

The Postdoctoral Advisory Committee Is Here For You
Archana Gopalakrishnan
In this first issue, we want to introduce and acquaint you with the services of the Postdoctoral Advisory Committee (PDAC) and how they affect your life. PDAC is comprised of postdoctoral fellows elected by the postdoc community (that’s you!). The members draft a budget that is supported by the School of Medicine (SOM) Dean’s office to put forth events that are fun, social, informative, and serve as a great resource for networking and career development. Typically, the PDAC, along with the Office of Postdoctoral Services (OPS), hosts one career event or workshop every month and an afternoon social event, ‘Coffee and Cookie’ hour. PDAC members also encourage other fellow postdocs to join them once a month at a local Baltimore venue for a social get together. Have you attended the workshop on ImageJ processing or career talks by experts from the field of Science Policy and Data Science? Have your baking and culinary skills been tested at the Annual Bake-Off and Thanksgiving Potluck? Or have you had the opportunity to meet and greet with postdocs from Johns Hopkins University during the joint social gatherings? If not, you are missing out on the extramural life of a postdoctoral fellow. The efforts of all postdocs are recognized annually, when the PDAC organizes the Postdoc Retreat to commemorate the National Postdoc Appreciation Week (NPAW) in September. Good food, great career development sessions, inspiring keynote speakers, and valued memorabilia have always served as the hallmark of the Postdoc Retreats.
COVID-19 has thrown us into challenging times filled with uncertainty and confusion. Despite this, PDAC continues to serve by adapting to the new normal of the virtual world. In-person networking and delectable Baltimore cuisine is something we might have to forego for a while, however, we can continue to learn about the different careers in science and network with fellow postdocs via Zoom. PDAC initiated the virtual seminar series by featuring FDA Reviewers on May 7th. On May 29th, PDAC hosted a virtual mini-series on Clinical Research, featuring a UMB alumnus. This is the start of the new normal that PDAC is learning to adapt to. Preparations for an exciting Annual Retreat is underway as PDAC recently confirmed their keynote speaker.
If you are curious about how these events will be held and want to learn more about PDAC activities, make your voice and opinion heard. PDAC elections are “Zooming” in now. Nominate yourself or a fellow postdoc for a position on the PDAC Executive board this month. If you have attended at least 1 monthly PDAC meeting this past year, you are eligible to apply to be the President or Vice President of the PDAC. Secretary and Treasurer are the other two positions that serve on the board. If multiple people are nominated for a position, you, the fellow postdocs can help to elect by virtual voting that will be open until June 10th. The new PDAC E-board will work alongside the current board in planning the 2020 Postdoc Retreat and take office in November. If you would like to contribute to PDAC but are unsure of your commitment level, PDAC recommends serving as a member-at-large. Remember, PDAC is made of the postdocs, for the postdocs. So, if you have an idea for a social event, career event, or workshop, just become a part of PDAC or email the serving members and bring the change you wish to see in the UMB postdoc community.
PDAC E-board serving for the year of 2019-2020:
|
President: Joanna Cooper |
Vice President: Ankit Dwivedi |
|
Treasurer: Aditya Jhajharia |
Secretary: Archana Gopalakrishnan |
Fighting COVID-19 with the Help of the Convalescent
Taissa Vila
 As of December 2019, a new acute respiratory syndrome (COVID-19) has been creating chaos in the world. COVID-19 is a devastating disease caused by a coronavirus, the same class of virus that causes the common cold. However, the “new coronavirus”, named SARS-CoV-2, is nothing like other coronaviruses we know. SARS-CoV-2, was first identified in a patient suffering from pneumonia in Wuhan, China and in a span of a month COVID-19 had reportedly killed almost 200 people within China and had quickly spread to the rest of the world. COVID-19 was recognized as a global pandemic in March 2020 by the World Health Organization (WHO) and, as of May 2020, over 5.7 million people have been infected and more than 350,000 have died from this disease (https://coronavirus.jhu.edu/). Along with two other coronaviruses related to outbreaks, SARS-CoV and the Middle East Respiratory Syndrome-Coronavirus (MERS-CoV), SARS-CoV-2 is the third coronavirus to provoke severe respiratory illness in humans (COVID-19) but is the first one to cause a pandemic.
As of December 2019, a new acute respiratory syndrome (COVID-19) has been creating chaos in the world. COVID-19 is a devastating disease caused by a coronavirus, the same class of virus that causes the common cold. However, the “new coronavirus”, named SARS-CoV-2, is nothing like other coronaviruses we know. SARS-CoV-2, was first identified in a patient suffering from pneumonia in Wuhan, China and in a span of a month COVID-19 had reportedly killed almost 200 people within China and had quickly spread to the rest of the world. COVID-19 was recognized as a global pandemic in March 2020 by the World Health Organization (WHO) and, as of May 2020, over 5.7 million people have been infected and more than 350,000 have died from this disease (https://coronavirus.jhu.edu/). Along with two other coronaviruses related to outbreaks, SARS-CoV and the Middle East Respiratory Syndrome-Coronavirus (MERS-CoV), SARS-CoV-2 is the third coronavirus to provoke severe respiratory illness in humans (COVID-19) but is the first one to cause a pandemic.
Despite having gone through two major outbreaks in the past (SARS, 2003 and MERS, 2012), coronavirus-specific antivirals are still missing in the market. As the pandemic spreads, effective treatments for COVID-19 are urgently needed however, there is no time to develop a “brand new” antiviral at this point. Therefore, biotechnology and pharmaceutical companies all over the world resorted to a repurposing strategy to find FDA-approved drugs that could be redirected for COVID-19 treatment. The list of possible treatments grows by the day and include the antiviral drug tested during the Ebola epidemic, Remdesivir (Gilead, US) and the antimalarial drug Hydroxychloroquine. So far, nothing has been proven effective and large randomized clinical trials are still pending.
With the number of cases increasing by the thousands every day and no specific treatments available to prevent or treat this disease, “convalescent plasma therapy” is being revisited as a viable and immediate option to alleviate the impact of COVID-19 in the population. The convalescent plasma approach is based on passive antibody therapy, where antibodies from the blood of someone who recovered from an infection (convalescent) are administered to protect or treat another person .1 The end goal is the same as vaccines, making antibodies against a specific infectious agent readily available, but the process is expedited by providing a patient with immediate immunity, skipping the weeks it takes for a person to produce their own antibodies. For several other diseases, passive antibody therapy is administered as pooled immunoglobulin preparations that contain high concentrations of antibodies. In contrast, plasma has been used emergently in epidemics where there is insufficient time or resources to generate immunoglobulin preparations. In fact, convalescent plasma treatment dates back to the 19th century, when it was used to treat patients during the Spanish Flu pandemic. More recently, it was successfully used during the 2009–2010 H1N1 influenza virus pandemic, as well as in the West African Ebola epidemic, in 2013. But what is encouraging about this approach is the high degree of success obtained using convalescent plasma during the two previous coronavirus epidemics, SARS and MERS.
Based on those historical successes, the convalescent plasma approach was proposed to treat COVID-19 patients by a group of researchers led by two Professors from the John Hopkins School of Medicine, Dr. Arturo Casadeval and the director of the Transplant and Oncology Infectious Diseases program, Dr. Shmuel Shoham. After contacting other researchers on the frontline of their hospitals, Dr. Casadevall and Dr. Shoham established a coordinated front to work on implementing convalescent plasma transfusions in the US. In fact, due to the high number of patients with severe COVID-19, things moved quickly and administering convalescent sera for COVID-19 treatment purposes is already being implemented.2,3,4,5
Currently, convalescent plasma is being proposed for the rescue of those already infected since giving them neutralizing antibodies could augment their immune response and increase successful outcomes. Although large studies are still ongoing, two small trials conducted in China have already shown convalescent therapy is well tolerated, able to neutralize the virus, and improved clinical symptoms in patients with severe COVID-19.6 These promising results indicate convalescent plasma can be used for immediate treatment of current COVID-19 patients. Additionally, convalescent plasma can also be administered to people considered at high risk for infection due to age, underlying medical conditions or those with high exposure risk for protection against future infection. In fact, passive antibody therapy is most effective when administered prophylactically or used in the beginning of symptomatic disease.
Earlier this month, the largest safety trial for convalescent plasma treatment to date was published online as a preprint (https://www.medrxiv.org/content/10.1101/2020.05.12.20099879v1). The study included 5,000 hospitalized adults presenting severe or life-threatening COVID-19 and confirmed the predicted safety of the treatment, setting the ground for a larger randomized trial. Even though efficacy was not the primary outcome evaluated in this trial, the authors discussed that hospitalized adults presenting severe or life-threatening COVID-19 treated with convalescent plasma showed a seven-day mortality rate of 14.9 percent, while reported fatality rate of COVID-19 among hospitalized patients and those admitted to the ICU ranges around 20 percent and 57 percent, respectively. Despite the non-zero mortality rate of plasma-treated patients, these results are encouraging considering the severity of disease in COVID-19 patients admitted to the ICU, including multi-organ failure, sepsis and/or other significant comorbidities. Large-scale randomized clinical trials will ultimately confirm the safety and efficacy of convalescent plasma therapy for COVID-19 and those are already being implemented.
Although the potential clinical benefit is still to be confirmed, convalescent plasma therapy could buy us the time we need to develop, test and deploy new targeted therapies, and eventually a vaccine against COVID-19.
References
[1] Casadevall A, Pirofski LA. The convalescent sera option for containing COVID-19. J Clin Invest. 2020. Epub 2020/03/14. doi: 10.1172/JCI138003. PubMed PMID: 32167489.
[2] Shen C, Wang Z, Zhao F, Yang Y, Li J, Yuan J, et al. Treatment of 5 Critically Ill Patients With COVID-19 With Convalescent Plasma. JAMA. 2020. Epub 2020/03/29. doi: 10.1001/jama.2020.4783. PubMed PMID: 32219428; PubMed Central PMCID: PMCPMC7101507.
[3] Duan K, Liu B, Li C, Zhang H, Yu T, Qu J, et al. Effectiveness of convalescent plasma therapy in severe COVID-19 patients. Proc Natl Acad Sci U S A. 2020. Epub 2020/04/08. doi: 10.1073/pnas.2004168117. PubMed PMID: 32253318.
[4] Ye M, Fu D, Ren Y, Wang F, Wang D, Zhang F, et al. Treatment with convalescent plasma for COVID-19 patients in Wuhan, China. J Med Virol. 2020. Epub 2020/04/16. doi: 10.1002/jmv.25882. PubMed PMID: 32293713.
[5] Sheridan C. Convalescent serum lines up as first-choice treatment for coronavirus. Nat Biotechnol. 2020. Epub 2020/05/03. doi: 10.1038/d41587-020-00011-1. PubMed PMID: 32358594.
[6] Bloch EM, Shoham S, Casadevall A, Sachais BS, Shaz B, Winters JL, et al. Deployment of convalescent plasma for the prevention and treatment of COVID-19. J Clin Invest. 2020. Epub 2020/04/08. doi: 10.1172/JCI138745. PubMed PMID: 32254064.
Has Social Distancing Made Science More Inclusive?
Sridevi Ranganathan
Social distancing measures to prevent the spread of COVID-19 have impacted academic and research progress, not just at the University of Maryland Baltimore, but globally. Pausing hands-on research, learning via online classes, and attending lab meetings and social hours virtually have become our new 'normal.' However, there may be a valuable lesson of inclusivity in this rather harrowing experience as well.
The American Association for Cancer Research (AACR) annual conference in 2019 had approximately 22,000 registered participants. Due to the pandemic, the AACR hosted a virtual conference in 2020. About 61,000 participants attended the online meeting securely from their home offices. Closer to home, there has been a 3 to 4-fold increase in attendance at the virtual career development events hosted by different departments at UMB. "This has been noted by others around the country in career development offices. Attendance has skyrocketed in the virtual format," says Jennifer Aumiller, Director of Pre and Postdoctoral Career Development, UMSOM. One might argue that disruption of research activity may have opened up calendars, allowing for the increased attendance. However, having a virtual option to attend conferences opens up a lot more than just schedules.
Online meetings come with some obvious advantages of time and cost-effectiveness. There is less time spent traveling, and therefore less time commitment required from speakers and attendees. The ability to share research and professional advice with minimal time commitment has also broken distance barriers, allowing the scientific community to benefit from expertise from all around the world. For example, the Microbiology and Immunology department at the UMB School of Medicine hosts a weekly seminar series. In the past two academic years, one out of fifty-nine invited speakers were from outside the United States. However, in its online format, just in May 2020, the department was able to host six speakers from outside the US.
E-attendance will allow for more diversity of participation as well. Attending an international conference is not cheap. The financial well-being of a lab may very well decide if the graduate students and postdocs in a lab may be able to attend a conference. Visa restrictions add another layer of complexity to attending international meetings. Thus, a virtual attendance option may allow participation and enhance the learning experience of scientists from different parts of the world.
It is also essential to recognize that academia is composed of people in diverse stages of personal and professional life. Researchers and academicians have additional roles as parents to young children or primary caregivers to elderly parents. An option to attend the conference virtually would enable at least a subset of these people to better balance their academic goals with their personal responsibilities, without sometimes having to choose one over the other.
The Americans with Disabilities Act, landmark legislation to provide equal opportunities to people with disabilities to participate in mainstream life in the US, was signed into law in 1990. According to the NSF, Americans with a disability only comprise about 9 percent of the scientific workforce. A lot needs to be done to make STEM fields seamlessly inclusive of people with disabilities. Along with including Universal Design concepts in learning, lab environments, and public conference venues, a provision to virtually attend meetings may be a viable option to consider as well.
Face to face interactions, collaboration, cultural exchange, and networking, are undeniable advantages of attending a conference in person. However, by forcing the scientific community to adapt to the digital age, social distancing has had an unintended and slightly paradoxical side effect. It has made science more inclusive, geographically diverse, and accessible. Moving forward, I expect that we will see more conferences with a hybrid format- both in-person and virtual attendance options to bring together the best of both worlds!

Image credit: https://unsplash.com/@cwmonty
In Conversation with Dr. Kirsten E.Lyke
Awadhesh Arya

COVID-19 vaccine research is currently being carried out at UMSOM Center for Vaccine Development and Global Health (CVD). Dr. Kathleen Neuzil, Director of CVD, and Dr. Kirsten E. Lyke are the investigators for this trial.
It was a great pleasure to chat with Dr. Lyke, an expert in the field of vaccine development, who is currently playing a leading role in the development of vaccine and clinical trials for COVID-19. Dr. Lyke is a clinical translational investigator at UMSOM with recognized expertise in malaria, tropical disease, and parasite immunology. She is the Director of the Malaria Vaccine and Challenge Unit and has been on the forefront for the development and clinical trials of vaccines for the Ebola and Zika viruses. She offers us some of her insights into the ongoing vaccine trials at UMB and what the future could look like.
Q1: What are the basic approaches your group is taking to develop vaccines for COVID-19?
We are taking a stepwise approach to maintain safety while accelerating development as quickly as we can. Currently, we are conducting a Phase I trial that starts with those aged 18-55 without COVID-19 risk factors. We will then move to, first, healthy 65-85 years old individuals and then 18-85 years old patients of all backgrounds and underlying conditions. We are open to working on many different vaccine constructs but want to devote resources to vaccines that have a reasonable chance of progressing to licensure.
Q2: What stage of COVID-19 vaccine development are we in, and what are the major challenges regarding this?
We are now at Phase I (safety and immunogenicity). We hope to move to Phase 2 by mid-summer. So far things have been going smoothly, which is not to minimize the amount of work that this vaccine effort has required and to ensure that the vaccine trial goes smoothly. I think that we will be successful developing a vaccine, but the production of such a vaccine will require a worldwide effort to provide enough product. Thus, we need to have many companies experience success and ramp up production of many successful vaccines.
Q3: After vaccinating a participant, how many days later do you expect to see an immune response? What readouts would make you feel confident that the vaccine is working?
We have a good idea of the antibody response that people who suffer a Covid-19 infection might mount. We will be measuring responses at many different time points following vaccination, as well as measuring how long these responses last over the course of 26 months. We measure responses as early as one week following vaccination and as long as 24 months. We can easily measure the total antibody response, but more sophisticated tests will be looking at the ability of the antibodies to neutralize the SARS-CoV-2 virus in vitro as well as a series of immunologic assays designed to better understand the immune response to the vaccine.
Q4: If another vaccine that is efficacious becomes available during the time frame of the current vaccine trial study, what would your recommendation be for the trial participants?
This is a hypothetical question, so I would respond hypothetically that we would always urge volunteers to receive any licensed vaccine that may protect their health. Participating in a trial should never introduce intentional safety risks. We are hoping that our effort will be one of many successful endeavors leading to a licensed vaccine. This is the only way to provide enough vaccine for the world at large, as quickly as possible.
Q5: We know that viruses have a tendency of antigenic drift continually over time, do you have any way to predict the next emerging strain out of SARS-COV-2? If so, how would you propose to deal with them?
This is a very good question. Fortunately, we have excellent researchers, such as Dr. Matthew Frieman (Department of Microbiology and Immunology at UMSOM), who can study the virus and provide our team with updated information. At a global level, funding needs to be returned to the surveillance teams that study emerging viruses. At present, we are working on forwarding an mRNA vaccine against COVID-19. The beauty of an mRNA vaccine is that the genetic code is something that can be produced rapidly, relative to more traditional vaccines. I would expect that this would apply to new strains of COVID-19, assuming the genetic mutations occurred within the proteins that make up the vaccine.
Q6: Can people expect to be immune once they’ve had the virus? Can the virus “reactivate”?
This is something that we will be studying. We are closely measuring antibody response, and the neutralizing antibody function in volunteers who will be followed over 26 months. We would like to measure response over the course of a future “second wave”. We simply do not know how long the immune response will last or whether immunity will be partial or complete.
Q7: How long do you expect the virus to be around? Will it be “seasonal” like the flu?
Mankind has effectively developed immunity to the 4 other circulating strains of coronavirus. SARS 1.0 and MERS were able to be suppressed after initial outbreaks. We don’t know the kinetics of SARS-CoV-2, but no one wants to wait until immunity develops, as this would require a great deal of suffering and death. As of today, there have been almost 5 million cases world-wide, and 319,213 deaths. As large as this is, it could be much worse. However, it may take some time for this strain to be a seasonal virus that we are able to tolerate without the quarantine measures required in these early days.
Q8: As an expert in the field of vaccine development, are you feeling more pressure than the days before outbreak of COVID-19 ?
I wouldn’t term it “pressure” so much as a sense of urgency that a vaccine is desperately needed. Our entire team is putting in long hours, weekends, and stepping up to get the job done quickly and without error. This is a team effort, and the entire CVD is working overtime to ensure that we conduct quality research into therapeutics and vaccines.
Q9: What gives you the most hope in this time? Has there been anything that has stirred you in a good way through this process?
I had experience as the Principal Investigator for the first Ebola vaccine trial and learned that it was possible to conduct trials and research in a safe but accelerated manner. We had another chance to ramp up vaccine development for Zika. We capitalized on those experiences for the COVID-19 vaccine effort towards this unprecedented pandemic. At every level, from the CVD, UMMC administration, industry, and the FDA, people have worked overtime to meet every deadline and accelerate the approval process of starting a trial of this magnitude. My experience has been one of complete cooperation and a shared sense of urgency. Additionally, I can speak to the comradery and teamwork at the CVD as well as within the Infectious Diseases division in the support of both the clinical duties as well as the research duties that we are all conducting. It’s very inspirational.
Q10: What are some long-term effects from this virus and this pandemic in general?
This is a complicated question. At an individual level, those who have suffered a prolonged hospitalization from COVID-19 may have a very long recovery process, if not permanent lung damage, depending on the severity of their illness. From an overarching perspective, many aspects of life will change. This is a virus that may be with us for a while. It will affect our work, school, and recreation in ways that we have yet to fully understand. I think that a second wave is almost certain, and it’s imperative that we begin to prepare to weather the days ahead. We cannot be caught as flat-footed as we have for this outbreak. Public health officials have been stating for years that a pandemic was not hypothetical but a certainty. This time we need the country and the world to cooperate and to prepare for the days ahead.
SPOTLIGHT ON: Dr. Chandler Sours Rhodes
Archana Gopalakrishnan
Dr. Chandler Sours Rhodes is a Clinical Research Specialist at the National Intrepid Centre For Excellence (NICoE). She began her career in clinical research while recruiting patients for her PhD thesis at UMB. After completing a short postdoc at UMB, she worked as an Associate at Booz Allen Hamilton that gave her the chance to be involved with DoD projects and therein, her entry into the government. She chats with us about her career journey from UMB to NICoE.
Q1: What does a typical day look like for you when you go to work? Has this changed a lot due to COVID-19?
A lot of my day involves sitting on my computer and reading articles and writing grants, IRB protocols, and manuscripts. Another part of my position is working with clinicians who are interested to get involved in research, so I spend a lot of time working with them and other junior research staff on developing projects and ideas. Also, since the NICoE is in walking distance of both NIH and the Uniformed Services University (military medical school), I can attend seminars and other research meetings. Since COVD-19, my professional life has changed from being in the office daily to working entirely remotely. While I do not miss commuting, working from home full time with an energetic two-year old certainly has its share of challenges. But like everyone else at this time, I have tried to make the most of the situation. While I have enjoyed the extra time, I get to spend with my family, I am also looking forward to getting back into the office and getting back into a semi-normal routine.
Q2: Do you get to interact a lot with clinical patients? If so, how has this experience been?
I do participate in some clinical interviews which has been a great experience to learn more about the specific military population that is seen at the NICoE. This was not new to me since my dissertation was in a clinical department (Diagnostic Radiology) and involved recruitment of traumatic brain injury patients from the hospital as well as conducting interviews and running the MRI scanner. Depending on the population that you will be working with, there may be some sensitivities to be aware of, but the best advice I have it to just be friendly and try to make them feel as comfortable as possible by explaining what they will be asked to do. It also helps to be able to explain the science of the project itself in a way that that makes sense to participants with various levels of education/different backgrounds.
Q3: What differences in the work environment did you encounter while moving from academia to government?
There are different pressures in these environments. As a research investigator for the government, there is not as much pressure to submit grants since my entire salary is supported by the government which is very different from academia. For me, any grants I submit are entirely to bring on new staff. In terms of work environment, the government is a little bit more formal in dress and in tone during meetings. But one of the biggest differences is that as both a contractor and a government employee, you are expected to work forty hours per week, not more, not less. As many of us know, this is not the expectation in academia where many researchers work much more than forty hours, so having set work hours and being able to leave work each afternoon and not be expected to be checking email in the evening is great.
Q4: Do you think it is necessary to have course certification in clinical research or training experience as a clinical research associate (CRA) to make a transition into this field?
I personally did not take any courses in clinical research, but I had experience in clinical research as both an undergraduate and graduate student since my dissertation involved clinical research in traumatic brain injury patients. From a knowledge/skills perspective, I think that research is research whether it is cell cultures, animals, or humans, but courses like this may be helpful to learn about some of the regulatory aspects of human subjects research (IRB, informed consent, etc). It also may be helpful to have these on a resume when applying for a clinical research position.
Q5: If not a Clinical Research Specialist, what would be your alternate career?
After my postdoc, I spent two to three years working for the US Air Force as well as Booz Allen Hamilton as a consultant before returning to an active research position for two years. I was still peripherally involved in research and it was a great experience to learn about the more administrative aspects of research as well as how large funding organizations (like the DoD) make decisions regarding what topics/projects to fund. In the future if I decide to move away from a research investigator/scientist role, a career in research administration would likely be my alternate career.
Q6: What was your most memorable moment as a postdoc at UMB?
I completed my postdoc in the same lab that I did my PhD in so not much changed for me professionally when I started my postdoc. But one of my most memorable experiences was volunteering at the National Postdoc Association’s annual meeting that was in Baltimore that year. It was a great opportunity to get to connect with postdocs in very different fields at UMB and learn more about their experiences and career plans.
Q7: What advice would you give a current UMB postdoc navigating through job search?
The advice I would give postdocs is to be flexible when looking for positions. I think that many of us complete postdocs because we have the goal of remaining in academia and transitioning from a postdoc position directly to a junior faculty position, but with faculty positions so limited, this goal is becoming increasingly hard to achieve. There are many alternative career paths that allow you to use the research and critical thinking skills you learned through your PhD and postdoc that can be just as fulfilling as academia (and may even provide a slightly better work-life balance).
How Has This Pandemic Shaped the Job Market?

Tramy Hoang
As if looking for a job wasn’t difficult enough, this pandemic has posed some additional challenges for those in the middle of or just starting this journey. Looking across the country, hiring statuses for universities range from temporary pauses to complete hiring freezes. This could mean previously announced job openings are being withdrawn, faculty searches are being put on hold, and job offers have even been rescinded. While the state of hiring varies, the one sure thing is that those looking for an academic job right now are in for some difficult times.
Take Dr. W for example. “My postdoc ends on August 31, sharp. There is no money to support me here anymore. I sent back up postdoc applications to couple labs, but they also don't know when they can hire a postdoc… [one] department wants to give me [a faculty] offer, however, they are waiting for dean's approval for an exception to hiring freeze. it is pretty tough for me, because I am very close to getting an offer from a dream job, but don't know whether I will officially get an offer… In short, I have no clue whether I will be even employed in September.”
Heidi Leonard, another recent postdoc, found herself in a similarly uncertain situation. She was a postdoc in a government lab and her fellowship will be ending this fall. However, her academic job search so far had been unsuccessful and she was uncertain about the job market in the next year. For these reasons, she reevaluated her plan and realized that an industry job can also help her achieve her goals. Ultimately, she decided to accept a position as the head of R&D for a start-up company. Her advice to those looking or planning to look soon is to be flexible. Where do you ultimately want to be? Are there multiple ways to get there?
Carina Collins has similar advice. She recently accepted a tenure-track position at a private university. In her job search, Dr. Collins had to factor in another challenge because her partner, a PhD, was also looking for a job. They had trouble finding faculty positions that would geographically work, so Dr. Collins expanded her search to non-faculty staff positions as well. “In order to be successful, you have to cast a wide net for jobs. I applied to all sorts of positions, academic and otherwise… I really had [to] think hard about what I wanted in my career... I think in addition to applying to a broad range of positions, you also have to think critically about what you want to achieve in your next career step and consider all of the options that are available. And more likely than not, there is more out there than you might think.”
As Dr. Collins found, while job prospects are lower, they are not impossible to find. One piece of advice for those currently looking is to do your research. If you can, contact the hiring department to get a better sense of their situation. Are they intending to fill the position soon? Are they accepting applications but are unsure what their timeline is? Whatever the situation, go in with all the information you can get to ensure that you are well prepared.
What about navigating the coveted job offer? Says Dr. Collins, “It was weird to have an “on-campus” faculty interview via video chat. Part of a faculty interview is ensuring that the applicant is a good “fit” for the institution, and I think it can be hard to discern that using digital communication.” While Dr. Collins was optimistic and ultimately accepted the offer, Dr. N is more hesitant. “In my case I am rushed to make a very fast decision on the offer without even having a chance to have a campus visit and meeting with other faculty in person. The rush is for fear that the position funding could be cut if not filled ASAP.” While there is no perfect solution in a situation like this, Karen Kelsky, an academic career consultant for The Professor Is In, advises that applicants sign a contract as soon as they can. Universities are also facing uncertain times and may want to fill positions while they still can. 1
A sector not facing quite a precarious a future is the biotech realm. Dr. Siddha Kasar, who is a team lead at Takeda in Boston, MA, has observed an increase in hiring at her company. In fact, she does not expect hiring to slow down as they have many products headed towards clinics in the coming years. This bodes well for the industry and suggests that the economic shift of this pandemic does not have a negative impact on biotech companies.
If anything, the job market within biotech companies look very promising as companies transition into projects related to SARS-Co-V-2/COVID19, whether this be developing diagnostic tests, searching for a vaccine, or developing/manufacturing medical equipment. According to Dr. Kasar, “Companies involved with COVID-19 related programs will grow; I suspect more and more companies will get involved in this area. Virology and vaccine research will be back in vogue.” Furthermore, a recent LinkedIn article reported hiring surges at the pharmaceutical companies GSK (<2500 positions), Takeda (2000 positions), and Catalent (>500).2 AstraZeneca is also looking to fill hundreds of roles in Maryland alone (Gaithersburg, MD) and are recruiting over 150 postdocs internationally.3 In that context, post-docs at UMB are in an ideal location as we are located in one of the largest biotech hubs in the country (Baltimore/DC region).4,5
And some final pieces of advice from Drs. Collins and Kasar: networking is key! Use this time to “virtual network” and send lots of cold emails. “Build new connections and nurture the ones you already have.” And since interviews may be virtual for the foreseeable future, practice speaking in front of a camera.
For postdocs at all stages of training, take advantage of this opportunity to further your training in all different aspects. This pandemic has provided a unique opportunity to attend virtual seminars and meetings that may not have previously been available or accessible. Closer to home, trainees can expect a regular schedule of virtual events hosted by our own Postdoctoral Advisory Committee, as well as the GPILS/OPS Career and Professional Development office and others (check out our list of upcoming events!).
- https://www.chronicle.com/article/The-Professor-Is-In-Stranded/248551.
- https://www.linkedin.com/pulse/heres-whos-hiring-right-now-andrew-seaman/.
- Astrazeneca.com/careers
- https://www.biospace.com/article/-top-cities-in-the-u-s-for-biopharma-stem-jobs/.
- https://www.genengnews.com/a-lists/top-10-u-s-biopharma-clusters-7/.
June Events
Careers in Science: Panel for Science Communications Careers - June 3rd 12-1 PM (Register Here)
Careers in Science: Panel for Industry Careers - June 9th 12-1 PM (Register Here)
The Postdoctoral Advisory Committee (PDAC) is holding their Executive Board elections! Voting ends June 10th. For more information, check your inbox for an email from PDAC
Scientific Research Paper Writing Class - 10-week workshop starting on June 10th
Careers in Science: Dr. Sergio Aguedo Mojica - Field Applications Scientist, Nexcelcom Bioscience. June 16th 12-1 PM (Register Here)
Careers in Science: Panel for Regulatory Science/Tech Transfer - June 23rd 12-1 PM (Register Here)
Careers in Science: "Building Your Career Path in the Pharmaceutical/Biotechnology Industry as a PhD" - Dr. William Soliman, Founder and CEO of the Accreditation Council for Medical Affairs (ACMA). June 30th 12-1 PM (Register Here)
*Please check your inbox for emails with more information and registration links for these events
Postdoc Achievements
Pavlos Anastasiadis
Erin Harberts
Erin Harberts received her PhD in 2014 from the UMB Microbiology and Immunology Department and is now completing her second year of postdoctoral training under the Signaling Pathways in Innate Immunity T32 in the laboratory of Dr. Robert Ernst. Her research in the Ernst lab focuses on studying the structure-activity relationship of Gram-negative bacterial lipid A, specifically investigating how alterations in structure contribute to innate immune activation via the TLR4 signaling pathway. This project includes the development of TLR4 ligands as vaccine adjuvants. One of the molecules with adjuvant-like activity that Dr. Harberts helped identify is currently funded for pre-IND enabling studies by the NIH that will move it towards potential clinical use. She was also recently selected as a 2020 Public Policy Fellow for the American Association of Immunologists which will provide her the opportunity participate in the public policy and legislative activities of this nationwide academic society. Being funded by the T32 has provided her a support network that fosters an atmosphere of collegiality and collaboration among current and past trainees. These interactions and the opportunity to expand her research community has encouraged her move toward independence through obtaining funds that she can use to continue her research endeavors.
Stephanie Hare.jpg)
Dr. Stephanie Hare completed her PhD at Georgia State University in Atlanta, GA, on resting-state functional MRI (fMRI) markers of symptoms of schizophrenia, with a focus on mechanisms of hallucinations. She joined UMSOM in August 2018, funded by a T32 fellowship in Multidisciplinary Schizophrenia Research (under the mentorship of Dr. Elliot Hong). Since arriving at UMSOM, Dr. Hare has continued to advance her training in fMRI approaches, published on neural correlates of increased allostatic load in schizophrenia (Psychosomatic Medicine), and modeled local and long-distance functional communication deficits related to an auditory perceptual disturbance in schizophrenia. Dr. Hare’s main T32 training goal has focused on transcranial magnetic stimulation (TMS) administration and analysis, with the ultimate goal to combine TMS with fMRI. She is working toward developing approaches to probe the neural mechanisms of symptoms of schizophrenia and to use TMS neuromodulation to treat symptoms that are resistant to current pharmacological treatment. Her participation is instrumental in an ongoing clinical trial on smoking cessation in patients with schizophrenia. Recent conference presentations include the Early Career Hallucinations Research Group Annual Meeting, London, U.K., and the Society of Biological Psychology in Chicago, IL. In Spring 2019, she was awarded the NIH Loan Repayment Award. Dr. Hare is currently in her second fellowship year.
If you would like to submit a postdoc we can highlight or a specific achievement from a postdoc, please fill out this form.
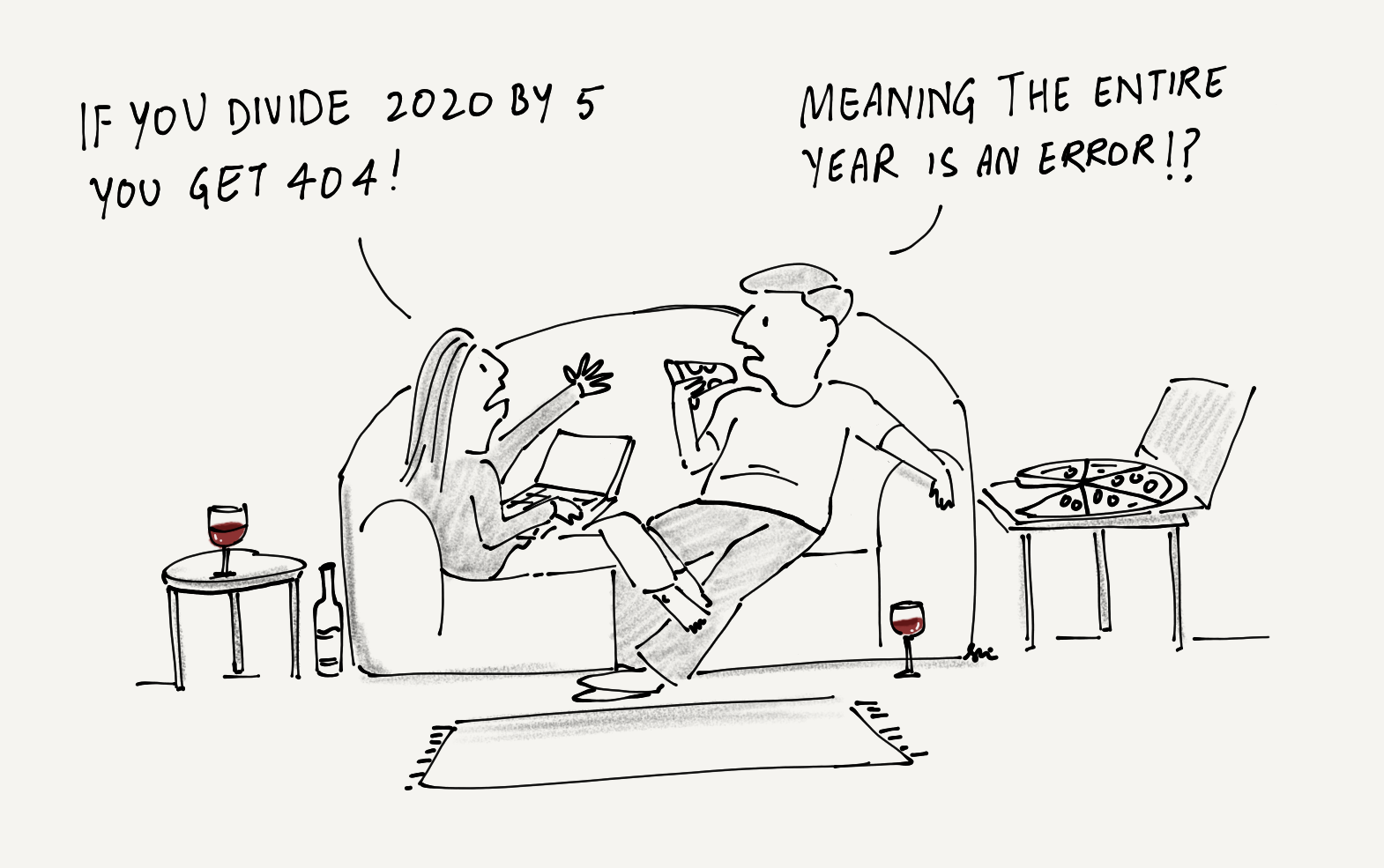
Nerdy Humor
Credit: Srinivas Ganesh
Check out Srinivas’s art at his Instagram handle @srinivas_ganesh
Are you looking to collaborate with an artist for your next project, Science or otherwise? Connect with Srinivas on LinkedIn!