Research in the Department of Otorhinolaryngology–Head and Neck Surgery
Our department is home to a vibrant and collaborative research community, spanning basic science, translational studies, and clinical investigations.
Nationally recognized as one of the top-funded otolaryngology research programs, we are dedicated to advancing knowledge and improving care for patients with ear, nose, and throat disorders.
Research Strengths
Our teams pursue a diverse range of projects with particular expertise in:
- Genetic hearing loss and inner ear biology
- Epigenetic changes driving head and neck cancers
- Tumor immunology and novel therapeutic approaches
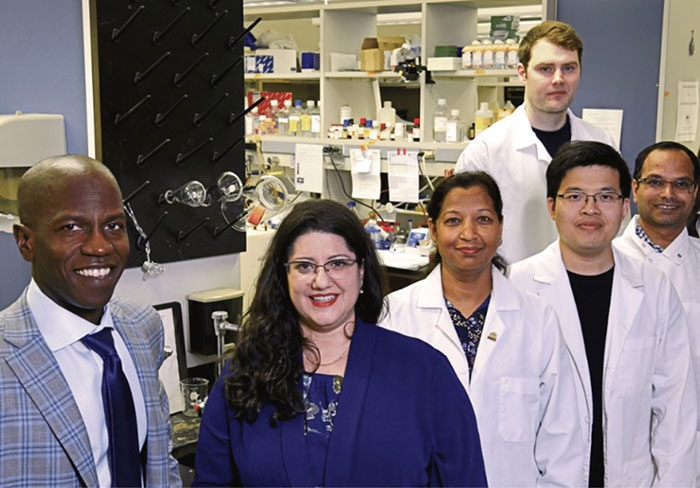
Collaborative Environment
Our basic science groups are housed in the state-of-the-art Health Sciences Research Facility III, where labs are co-located to encourage daily interaction, joint lab meetings, and shared journal clubs. This collaborative structure fosters innovation and accelerates discovery.
Multidisciplinary Partnerships
The Department of Otorhinolaryngology has strong alliances with colleagues across the University of Maryland, including the Departments of Biochemistry & Microbiology, the Institute for Genome Sciences, and the Program for Personalized and Genomic Medicine. These partnerships create a multidisciplinary network that bridges fundamental science and patient-centered research, driving meaningful translational advances.
Faculty Research

Zubair Ahmed, PhD
The team of Dr. Ahmed is focused on understanding how the retinal and inner ear sensory epithelia develop and function. Dr. Ahmed’s research interests consist of: (1) Inherited human disorders of retina and inner ear, like Usher syndrome (USH); and (2) Oculocutaneous Albinism (OCA). The studies under investigation are designed to answer the following broad questions: What are the precise mechanisms of various forms of hearing and vision dysfunction? What are the genetic factors that determine light sensitivity? How do the pathogenic mutations in disease-causing genes affect the ear, eye and skin structure and function? And which molecules or genetic factors can exacerbate and/or mitigate the effects of disease-causing genes? For these studies, families segregating inherited USH and OCA are being collected. Mutant mouse and zebrafish models have been developed, and we evaluate them to understand the function of new proteins. Functional analysis of the newly identified genes associated with deaf-blindness and OCA promises new insights into the molecular mechanisms of vision and auditory development and functions, and will facilitate the rational design of potential therapies.

Daria Gaykalova, PhD
Dr. Daria Gaykalova heads the translational laboratory, which defines the functional role of epigenetics in transcriptional regulation of cancer development and progression, mutational burden, and immunological landscape in tumors. The goal of her lab is to discover tumor-type-specific epigenetic and targeted treatments, particularly for tumors that lack disease-specific treatment protocols, such as head and neck squamous cell carcinoma (HNSCC). Her recent studies suggest that the chromatin landscape is the primary driver of viral integration, cancer-specific gene expression, and alternative splicing landscape in HNSCC. These data indicate that the combination of epigenetic treatment with the inhibitors of oncogenic and alternative protein expression is especially potent for cancer treatment. Her group adopted diverse high-throughput analyses for various preclinical models and primary patient samples, bridging high-throughput data analysis, robust experimental validation, and drug treatment. The research is funded by multiple sources, including NIH awards.

Ronna Hertzano, MD, PhD
Dr. Hertzano’s research laboratory uses cell-type-specific approaches to (1) define the key regulatory events that lead to cell type-specific differentiation — specifically, identification and characterization of transcriptional cascades that lead to hair cell terminal differentiation and survival as a crucial step in developing regenerative treatments for hearing loss; and (2) defining the molecular events as a result of acquired and noise-induced hearing loss to develop novel approaches for prevention and treatment of these problems. The team uses cell-type-specific genomic approaches in mice and zebrafish, followed by validation using genetically engineered animal models and classic experimental and developmental biology techniques.

Amal Isaiah, MBBS, DPhil, MBA
Dr Isaiah’s research interests span the domains of (i) innovative analytic tools, (ii) children’s brain development and neurocognitive outcomes, and (iii) biomedical device development. His group uses advanced statistical models, visualization techniques, and machine learning to dissect long-held associations and causal conclusions within large heterogeneous datasets with application to children’s health. Of interest is the domain of pediatric sleep disordered breathing, where he has published extensively on the use of causal mediation models to better identify the extent of the relationship between the severity of upper airway obstruction on neurobehavioral outcomes. He is closely involved in the Adolescent Brain Cognitive Development Study, the largest study of brain development in children, in which he studies the impact of environmental stressors on brain development. Lastly, he continues to develop, in collaboration with scientists at the University of Maryland, College Park, medical technologies specifically with application to children’s health and respiratory sensing.
Adam C. Kaufman, MD, PhD
Dr. Adam Kaufman leads a translational research program focused on understanding the biology and improving the treatment of ear and skull base disorders. His work spans molecular, clinical, and computational approaches, with active projects investigating the immune basis of recurrent otitis media, developing preclinical models of chronic suppurative otitis media, and establishing donor-derived temporal bone and inner ear tissue resources to advance hearing research. Dr. Kaufman also directs efforts to integrate large-scale clinical datasets with machine-learning algorithms to generate predictive models of hearing outcomes, aiming to personalize care and improve patient decision-making. His group is advancing novel clinical trials in areas such as hearing protection during chemotherapy, intranasal vaccination to study mucosal immunity, and innovative vaccine platforms for viral pathogens. Through this work, his team bridges basic and clinical science, organoid and animal models, and data-driven discovery, with the goal of developing new diagnostic and therapeutic strategies in otology and neurotology. His research is supported by institutional and federal funding sources.

Saima Riazuddin, PhD, MPH, MBA
Dr. Riazuddin’s team is focused on understanding the molecular and genetic basis of hearing impairment. This is done by ascertaining large human families segregating hearing loss and through genetic screening; disease-causing mutations are identified in these families. The identified mutations are further studied by analyzing the orthologous mutant mouse models, which are evaluated for developmental, structural and physiological defects of the inner ear. This will help us better understand the mutated genes and the underlying molecular mechanism of the hearing process. Identification of such genes will help in early and more accurate diagnosis for certain forms of hereditary hearing impairments. The lab uses various approaches ranging from genetic analysis of human DNA samples to screen and identify the candidate genes, to molecular biological approaches to determine the expression of the gene under study at the protein /RNA level. To further study the target genes, different model systems are exploited, which include but are not limited to mouse, Zebrafish, etc., where expression, localization and morphology of the inner ear is compared to wild type controls.
Rodney J. Taylor, MD, MPH
Dr. Taylor is a surgeon-scientist whose clinical practice is dedicated to the comprehensive care of patients with head and neck pathology. He has established an academic-tertiary practice with patients referred for complex surgical management of head and neck malignancy, skull base tumors, thyroid cancer and parathyroid tumors, and sino-nasal disease. His research goals are aligned with his clinical objectives: to improve the survival of patients with head and neck cancer. His lab has focused on factors impacting immune-cytotoxicity and immune-tolerance. His lab has extensive experience working with squamous cell cancer of the head and neck (SCCHN) cell lines and murine xenograft tumor models. Based upon findings from his laboratory, he initiated and completed a multi-institutional clinical trial evaluating the impact of NK FcγRIIIa polymorphisms on antibody-based therapy for SCCHN. This work has provided insight into which patients best benefit from antibody-based therapy for SCCHN. His lab has forged a collaboration with Dr. Zalzman’s lab, and he has successfully established murine models to study head and neck cancer stem cell immortality mechanisms using xenografts. Additionally, the two labs have combined to harvest adult mesenchymal stem cells to both improve their long-term survival in culture while preserving their differentiation potential, ultimately facilitating advancements for regenerative medicine.

Michal Zalzman, PhD
Dr. Michal Zalzman is a molecular cell biologist and a stem cell expert who made significant discoveries related to a novel mechanism triggered by ZSCAN4, controlling replicative lifespan of embryonic stem cells. Her studies are published in leading journals such as Nature, Cell Stem Cell, Stem Cell Research and Therapy, Oncogene and PNAS. Using the technology developed in the Zalzman Laboratory, her team establishes novel protocols for 3D-printed adult-stem cell implants for regenerative medicine and bone reconstructive surgeries. Further, the team develops novel stem cell therapies for neurodegenerative diseases. In collaboration with Dr. Rodney Taylor, her laboratory further studies the human ZSCAN4 mechanism components and function, with the goal to develop these targets as new strategies for cancer precision medicine. Dr. Zalzman and her team holds multiple patents and patent applications based on her work, and her research is funded by major federal grant awards from NIAMS and NINDS/National Institutes of Health.

