Vol. 2 Issue 1
Please select a topic or scroll down the page:
Letter from Chair | Promoted Faculty | Clinical Spotlight |Research Spotlight | Welcome New Faculty | Grants | Culture/Diversity | Philanthropy | Service Excellence | Resident Updates | Archive

Letter from the Chair
Happy spring and welcome to the third edition of the Maryland Dissector. Closing the door on another year challenged by the COVID-19 pandemic, I encourage you all to look forward to the brighter future ahead. Our department continued to thrive and grow despite the impact felt throughout the medical community over the last year. Moving toward another new normal in our pre-pandemic way of life, I challenge you to maintain efforts to harness the strength and resilience the epidemic taught us and leverage it towards increasing excellence daily.
Highlighting steadfast growth within the Department's research efforts is essential as we approach the midway point of the academic year. One of the biggest departmental FY21 goals was to rank in the top 10 Blue Ridge Institute for Medical Research rankings. It is my pleasure to share that the Department exceeded this goal and expectations! In the past several years we moved from 26th in FY18 to 18th in FY19 then 12th in FY20 to 9th in FY21. This accomplishment was possible with our faculty and staff's unwavering dedication to continued research and scholarly work. Over the last few months, the Department received several NIH R01s, a 7-year R35 from the National Institute of Allergy and Infectious Diseases, a Patient-Centered Outcomes Research Institute, and awards from several foundations and non-profits, including the American Heart Association.
Another significant achievement in the Department of Surgery was one for the history books. On January 7, 2022, Maryland Medicine performed a groundbreaking cardiac xenotransplant. This surgical endeavor, a culmination of decades of research by Dr. Bartley Griffith and Dr. Muhammad Mohiuddin, demonstrates budding possibility in revolutionizing the field of transplant surgery forever. With a national average of 17 people dying daily while waiting for an organ transplant, this surgery offers the potential for a giant first step in alleviating the organ shortage crisis.
I remain confident the Department of Surgery continues to achieve great things as we navigate another year of change. Please continue to care for yourselves, your families, and your colleagues. Brighter days ahead.
Best wishes,
Christine Lau, MD, MBA
Recently Promoted Faculty
Faculty were promoted to the titles listed below their name.
Cherif Boutros, MB, CH.B., MSc, FACS
Professor, General & Oncologic Surgery

Margaret Lauerman, MD
Associate Professor, Trauma Surgery

Jonathan Morrison, MB, CHB, PhD, FRCS, FEBVS
Associate Professor, Trauma Surgery

Khanjan Nagarsheth, MD, FACS, MBA
Associate Professor, Vascular Surgery

Joseph Rabin, MD, MS, MIA FACS
Associate Professor, Trauma Surgery
Rawn Salenger, MD
Clinical Associate Professor, Cardiac Surgery, St. Joseph Medical Center

Mohummad Minhaj Siddiqui, MD, FACS
Associate Professor, Urology Surgery

Eric D. Strauch, MD
Professor, Pediatric Surgery
Clinical Spotlight

Eugene Schweitzer, MD
Professor of Surgery, Division of Transplantation
New Dialysis Access Program
Eugene Schweitzer, MD, Professor of Surgery, Division of Transplantation and the Division of Vascular Surgery developed a new dialysis access program to improve the care for patients with end stage renal disease in the Baltimore metropolitan area. The program offers dialysis access surgical services and consults at Midtown Medical Center, University of Maryland Medical Center and in the community. Additionally, a variety of dialysis access maintenance procedures are performed in the Maryland Vascular Center at Redwood. Through the Maryland Vascular Center, Dr. Schweitzer and the team provide same-day services and transportation for patients to and from local dialysis units for their urgent fistulagrams and thrombectomies.
The surgeons in the program perform:
- Mechanical and chemical thrombectomy
- Angioplasty
- Stenting of fistulas and grafts
- Tunneled dialysis catheter and implantable infusion port placement
- Pre-op central thoracic venograms using contrast, CO2, and intravascular ultrasound
Point-of-care diagnostic ultrasound exams and vein mapping are available in the on-site Vascular lab. The program’s primary goal is making care for this patient population as convenient and accessible as possible.
Dr. Schweitzer maintains ongoing interest in dialysis access and performed thousands of dialysis access surgeries in his impressive 30-year tenure at the University of Maryland as a kidney and pancreas transplant surgeon. “Patients with kidney failure who are waiting or ineligible for a kidney transplant must be on dialysis to stay alive. The dialysis access devices can be a great source of suffering for patients, especially when creation and maintenance are handled by healthcare providers with only a shallow interest in the field. We minimize the risk of technical complications such as early thrombosis or nerve injury through meticulous surgical technique” stated Dr. Schweitzer.
The Dialysis Access Program aims to avoid patients’ suffering by providing state-of-the-art care from experienced University of Maryland attending surgeons, and timely, personalized service by a friendly, respectful staff.
Research Spotlight
Patient Preferences in the Treatment of Thyroid Disease

Yinin Hu, MD
Assistant Professor of Surgery
Division of General and Oncologic Surgery
Yinin Hu, MD, Assistant Professor of Surgery, Division of General and Oncologic Surgery, and his team are researching patients’ perspectives on treatments for thyroid diseases, including Graves’ disease and benign and cancerous thyroid nodules. He focuses on treatments including surgery, active surveillance, and radiofrequency ablation. The three treatments are most likely equivalent in terms of cancer survival, but active surveillance and radiofrequency ablation do not have extended follow-up yet, so it is not definitive.
Dr. Hu personalizes the best possible treatment plan for patients based on the individual’s preferences and values. “Recent research has shown that quality-of-life surveys provide inconsistent estimations of treatment value in thyroid disease. Our approach will be to use a direct, preference-based method to measuring treatment value, and to validate this approach across different types of participants” stated Dr. Hu. By collecting data from patients, the general population, and healthcare providers, Dr. Hu hopes to identify differences in value perception that may originate from addressable knowledge gaps. One-time surveys/questionnaires help describe patient preferences and perceptions and are not a prospective clinical trial.
The project collaborators include the Departments of Surgery, Pharmaceutical Health Services Research, and the division of Endocrinology. Project conception occurred in Fall 2020.
Welcome New Faculty
Chandra Bhati, MD
Professor and Director of Liver Transplantation, Division of Transplantation
Dr. Bhati completed a one-year Clinical Fellowship in Transplant Surgery and a three-year General Surgery residency from the University of Illinois Medical Center in Chicago.
Gregory Bittle, MD
Assistant Professor, Division of Thoracic Surgery
Dr. Bittle received his medical degree from the University of Maryland School of Medicine graduating Cum Laude and Alpha Omega Alpha. He also completed his Cardiothoracic Surgery residency at the University of Maryland.
Meghan Garstka, MD, MS
Assistant Professor, Division of General and Oncologic Surgery
Dr. Garstka received her medical degree from Tulane University School of Medicine in New Orleans, LA. She completed her General Surgery residency with a one-year General Surgery research residency at Tulane University School of Medicine.
Jeanwan Kang, MD
Associate Professor, Division of Vascular Surgery
Dr. Kang received her medical degree from Harvard Medical School and completed her residency at Massachusetts General Hospital.
Ann Kim, MD
Assistant Professor, Division of Vascular Surgery
Dr. Kim completed her medical degree, General Surgery residency and Vascular Surgery Fellowship at University Hospitals Cleveland Medical Center/Case Western Reserve University.
Grants
The Blue Ridge Institute for Medical Research has just published the Ranking Tables of NIH Funding to US Medical Research for 2021. Under the Clinical Science Department, Surgery, the University of Maryland Baltimore (UMB) has moved in its ranking to 9, with a total 2021 NIH award dollars recorded as $13,629,398. The Department ranking in 2020 was 12 and recorded NIH award dollars as $12,328,770.
Blue Ridge Institute for Medical Research NIH Funding - SOM Surgery Ranking 14 Year History
| Year | Rank | NIH Award Dollars |
|---|---|---|
| 2021 | 9 | $13,629,398 |
| 2020 | 12 | $12,328,770 |
| 2019 | 18 | $8,052,916 |
| 2018 | 26 | $5,361,931 |
| 2017 | 23 | $5,144,784 |
| 2016 | 20 | $4,405,093 |
| 2015 | 22 | $4,575,010 |
| 2014 | 21 | $4,380,754 |
| 2013 | 24 | $3,844,771 |
| 2012 | 23 | $4,300,787 |
| 2011 | 8 | $7,103,672 |
| 2010 | 9 | $8,459,942 |
| 2009 | 11 | $8,404,738 |
| 2008 | 10 | $8,254,332 |
Culture/Diversity
Students Begin Renaissance Curriculum in May Clinical Rotations
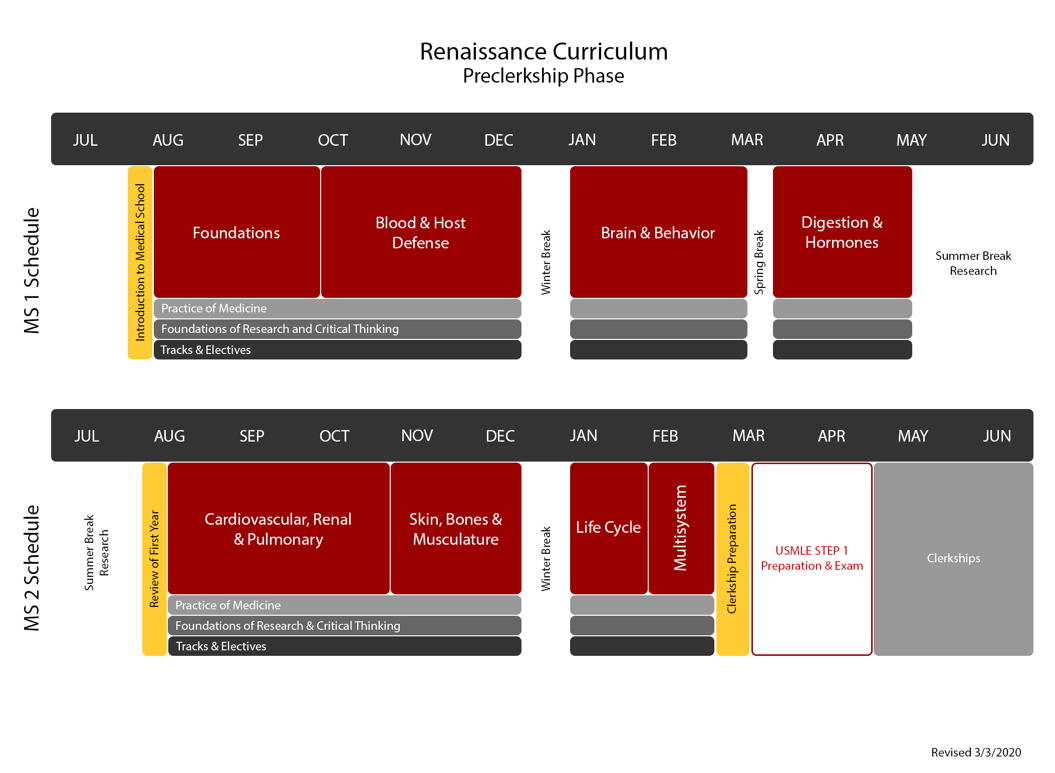
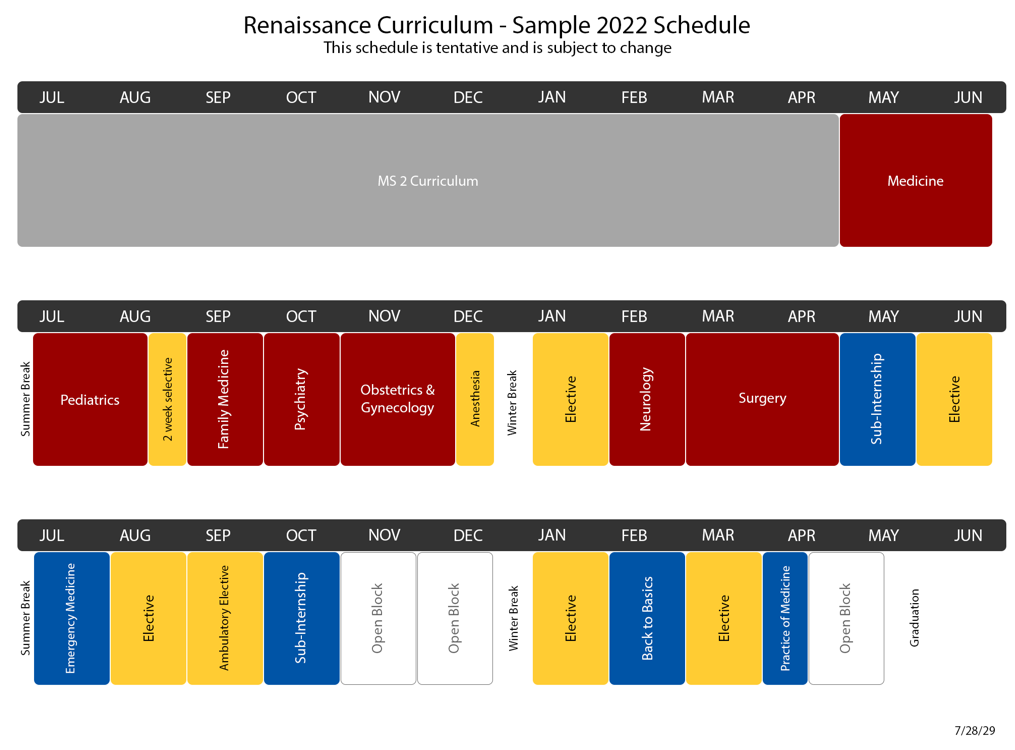
In August 2020, UMSOM launched a new medical school “Renaissance Curriculum” with students beginning their clinical rotations in May.
The biggest changes:
- In the first year, normal and abnormal processes taught together.
- The preclerkship classes reduced to 68 weeks, rather than 73 weeks to allow earlier clinical exposure.
- The school changed to an Honors, High Pass, Pass grading system in all years.
- Clinical clerkships expanded to 44 weeks from 40 weeks.
- Required clinical clerkships streamlined to allow for greater flexibility and more electives in the third year.
- The USMLE program changes score reporting for Step 1 from a three-digit numeric score to pass/fail outcome in 2022. A numeric score continues for Step 2 Clinical Knowledge (CK).
- Fourth year includes a required “back to basics” experience, tailored towards their career path.
Every year, the AAMC issues a questionnaire to all graduating medical students in the country. Known as the GQ study, it reports on national percentile responses as compared to your medical school. Our UMSOM graduates of 2020 reported that the quality of their surgical clerkship teaching was 86% good or excellent (medicine was 97%). Students reported that resident teaching was 77% “good to excellent” and surgery attending teaching was 69%.
How can we improve teaching? Eric Strauch, the clerkship director for the third year Surgery rotation, is also an officer of UMSOM’s Medical Education Leadership Academy and a winner of the Pass and Susel Faculty Educational Excellence Award. He points out that “in this age of rapidly changing technology and communication, access to data, facts, and information is readily available to anyone with a computer or phone. We need to focus our education on using the information available to interpret the data and think critically and clinically. Focusing on formulating accurate differential diagnoses, quality assessments and clinically effective plans is paramount to being an excellent physician.” Studies show that students rate increased contact with surgical teaching staff highly, that they value increased mentoring and positive role models that encourage communication. Additionally, part of the UMSOM promotion process includes a documented teaching portfolio.
“The good teacher explains. The superior teacher demonstrates. The great teacher inspires.” ― William Ward

Left to right: Dr. Daniel Maluf, Danielle and Johnny Class
Philanthropy
Giving Back While Moving Forward
HOW THE CLASS FAMILY CONTINUES TO TURN TRAGEDY INTO TRIUMPH
If you lived in Maryland in 2013, the name ‘Gavin Class’ is probably quite familiar. In August 2013, Gavin Class, a Towson University football player, collapsed at practice due to exertional heatstroke. Upon arrival at the R Adams Crowley Shock Trauma Center, his life-threateningly high body temperature lead to a cascade of medical problems that would make any person’s head spin, including the need for a liver transplant.
“We were thrown into it in just a couple of days”, Gavin’s mother, Danielle says, remembering how quickly everything happened. Gavin received the liver transplant he needed at the University of Maryland Medical Center (UMMC) and continues to thrive today.

Creating the scholarship was just the beginning. In 2020, the YOLT Foundation generously donated $15,000 to the University of Maryland Medical Center to launch a lodging fund. The fund benefits transplant patients and their families during the transplant process to offset the cost of lodging, meals, etc. Danielle said the inspiration to create the lodging fund came from seeing patients whose families’ financial challenges prevented them from visiting their loved ones. Since its creation, the lodging fund helped three families with support during their journey through transplants.
In their most recent endeavor, the YOLT Foundation teamed up with Dr. Daniel Maluf, a transplant surgeon with more than 19 years of experience in clinic and translational research, to fund the start of an Artificial Intelligence (AI) Program here at UMMC. Danielle remembers how long Gavin was in the hospital after his transplant and the testing that played a part in his recovery. The AI Program hopes by providing post-operative transplant patients with a tablet and an Apple Watch, patients can go home faster while still accessing continuous monitoring, similar to what they receive in the hospital. This allows patients to safely continue their recovery in a more comfortable environment and reunite sooner with their loved ones.

Service Excellence
Implementing a Daily Huddle
In FY22, the department averages a score of 93 for Staff Working Together when our goal is 95.3. One suggestion to help increase your score, and improve the patient experience, is to meet with your clinical team (Medical Assistant, Medical Secretary, Nurse/NP/PA, etc.) prior to the start of a session. These brief conversations prepare your team to proactively plan for patient needs on a daily basis. Best practices establish a huddle structure which address patients with special needs, potential scheduling issues, equipment/resource requirements, and any other information deemed necessary. Patients gain a higher level of confidence in you and your practice as they see information and instructions flowing smoothly among the team. Providing seamless care coordination ensures a positive experience for your patients and assists in reaching your goals.




